Tips for billing Expedited Comprehensive Consultations to WorkSafeBC
Physicians with a Royal College of Physicians and Surgeons of Canada specialty and family physicians with areas of expertise can bill WorkSafeBC for Expedited Comprehensive Consultations. Data from WorkSafeBC show that some of these physicians are still experiencing payment delays or rejections for these consultations. Below are tips to make the billing process smoother, restated and updated from when we covered this topic in the BCMJ in 2022 [64:249].
When to bill for an Initial Expedited Comprehensive Consultation
If you are an applicable physician, you may bill an Initial Expedited Comprehensive Consultation fee when:
- You receive a new referral for consultation from a referring physician or from WorkSafeBC (on behalf of the referring community physician), including when the consultation occurs because of an emergency.
- More than 6 months have elapsed since you last saw the injured worker and you have received a new referral.
The Initial Expedited Comprehensive Consultation report must be received by WorkSafeBC within 15 business days of you receiving the referral.
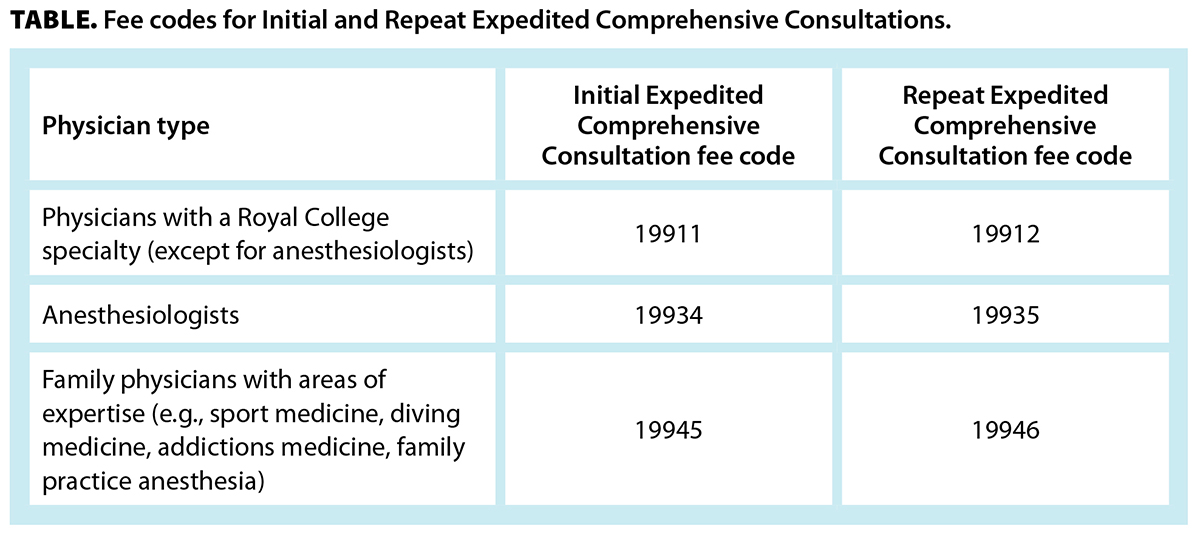
The fee code to use depends on whether you have an area of expertise or a Royal College specialty and what your specialty is [Table].
When to bill for a Repeat Expedited Comprehensive Consultation
A Repeat Expedited Comprehensive Consultation fee may be billed when:
- You complete a repeat consultation within 12 weeks of the Initial Expedited Comprehensive Consultation.
- The Repeat Expedited Comprehensive Consultation fee code has not been billed already.
Only one Repeat Expedited Comprehensive Consultation fee is billable following the Initial Expedited Consultation fee. Any other repeat consultations should be billed using the appropriate MSP consult fee code.
The Repeat Expedited Comprehensive Consultation report must be received by WorkSafeBC within 5 business days of the consultation [Table].
Submitting the consult report: Steps to avoid payment delays and rejections
When any Expedited Comprehensive Consultation fee code is invoiced to WorkSafeBC, the system automatically searches for proof of a consult report. If the system cannot find the report, the invoice is reviewed manually by WorkSafeBC staff, which may cause payment delays. If WorkSafeBC staff cannot find the appropriate consult report, payment may be rejected.
All Expedited Comprehensive Consultation fee codes include the physical examination and the report. No other fees should be billed for the report.
You have two options for cover sheets when you fax your consult report to WorkSafeBC at 1 888 922-8807:
- Use the Physician Consult Report Fax Cover Sheet (Form 83D556) found on www.worksafebc.com. This cover sheet tags and identifies your report for easier and more timely payment.
- Use your own cover sheet, clearly noting “Consult Report” and the worker’s claim number. You can get the claim number from the referring physician or the worker.
If you choose not to use a fax cover sheet, mark your consult reports with the title “Consult Report.”
Additional reminders:
- Clearly document the worker’s claim number on all pages of your report.
- Send the consult report as soon as possible. It must be received by WorkSafeBC before your billing.
- Ensure your documentation is legible. We recommend typing reports.
- Fax your consult report separately from your operative report. This ensures they each get matched to your billing.
Consult reports must be comprehensive and documented in keeping with professional standards (according to the College of Physicians and Surgeons of British Columbia’s Medical Records Documentation Practice Standard).
Finally, ensure any consult report transcribed by a hospital has been faxed to WorkSafeBC.
Seeing workers before WorkSafeBC has accepted their claim
If a worker makes a WorkSafeBC claim and we have not yet accepted or denied it (WorkSafeBC calls this “pending” status), you do not need to wait for approval from WorkSafeBC to expedite the initial consult. You can check if a claim is accepted, denied, or pending by using the tool at https://pvc.online.worksafebc.com.
If a patient has a pending claim, please see them as soon as possible to ensure the consultation is completed and the report is received by WorkSafeBC within 15 business days to meet timelines for payment. For these pending claims, subsequent visits (including Repeat Expedited Comprehensive Consultations) may not be covered by WorkSafeBC.
More information
Details on billing Expedited Comprehensive Consultations can be found in the Physicians and Surgeons’ WorkSafeBC Services Reference Guide at www.worksafebc.com/en/health-care-providers/provider-types/physicians.
—Patrick Wong
Quality Assurance Supervisor, WorkSafeBC
—Waqar Younas, PhD
Senior Analyst (Advocacy Operations), Doctors of BC
hidden
This article is the opinion of WorkSafeBC and has not been peer reviewed by the BCMJ Editorial Board.
 |
| This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. |