The value that a team-based approach brings to family practice
Team-based primary care offers many benefits to patients, physicians, and others, including enhanced access to care, increased comprehensive care, stronger relationships with patients, and improved satisfaction.
For physicians who are able to access the services of primary care network–funded team members or who independently hire allied health providers or nurses for their clinics or other primary care settings, the Family Practice Services Committee’s (FPSC’s) Practice Support Program (PSP) offers coaching, programs, and financial assistance to strengthen and optimize team-based primary care.
Improving comprehensive family practice
In New Westminster, Dr Paras Mehta has seen measurable improvements in accessible, comprehensive, and coordinated care in his clinic for patients who need rapid follow-up after a visit to the emergency department. Dr Mehta and his team—including medical office assistants, a registered nurse, a pharmacist, and a community health nurse—recently completed a quality improvement project focused on improving access and care for these patients.
The clinic was averaging six calls per week for patients discharged from the emergency department, all being seen by Dr Mehta. He approached the PSP for coaching support to help enhance communication within his interdisciplinary team, clarify roles, and increase coordination with health authority home care support teams and resources.
Since January 2024, the PSP’s team-based care coaches have used patient panel and electronic medical record (EMR) data to help more than 200 family physicians and 750 team members. The PSP also collaborates closely with local divisions of family practice and primary care networks to address community priorities and implement practice-based quality improvement projects.
Now at Dr Mehta’s clinic, staff connect patients postdischarge with the registered nurse, who determines each patient’s specific needs: an appointment with Dr Mehta, connection to the health authority’s home care support team, or a call with the pharmacist.
Dr Mehta says this approach has also significantly improved postdischarge support, particularly for frail patients. The team can address patients’ immediate needs more quickly, and patients receive coordinated follow-up from both home health and the clinic, reducing their stress. According to Dr Mehta, staff feel more confident about ensuring patients will get timely access to care and are less worried about patients falling through the cracks because their team is now communicating regularly.
Although the pharmacist and community health nurse are not located within the clinic, they can access Dr Mehta’s EMR and add notes directly in patient charts. This provides valuable context for clinical decisions and facilitates more efficient team communication and collaboration.
Dr Mehta says the PSP coach, Ruthann Robinson, helped the team create a workflow with direct communication, regular team meetings, and the ability to connect in real time. Rather than simply sharing space, their team is now working to each member’s strengths. They support and rely on each other to deliver the best care possible.
The value of team-based care, in numbers
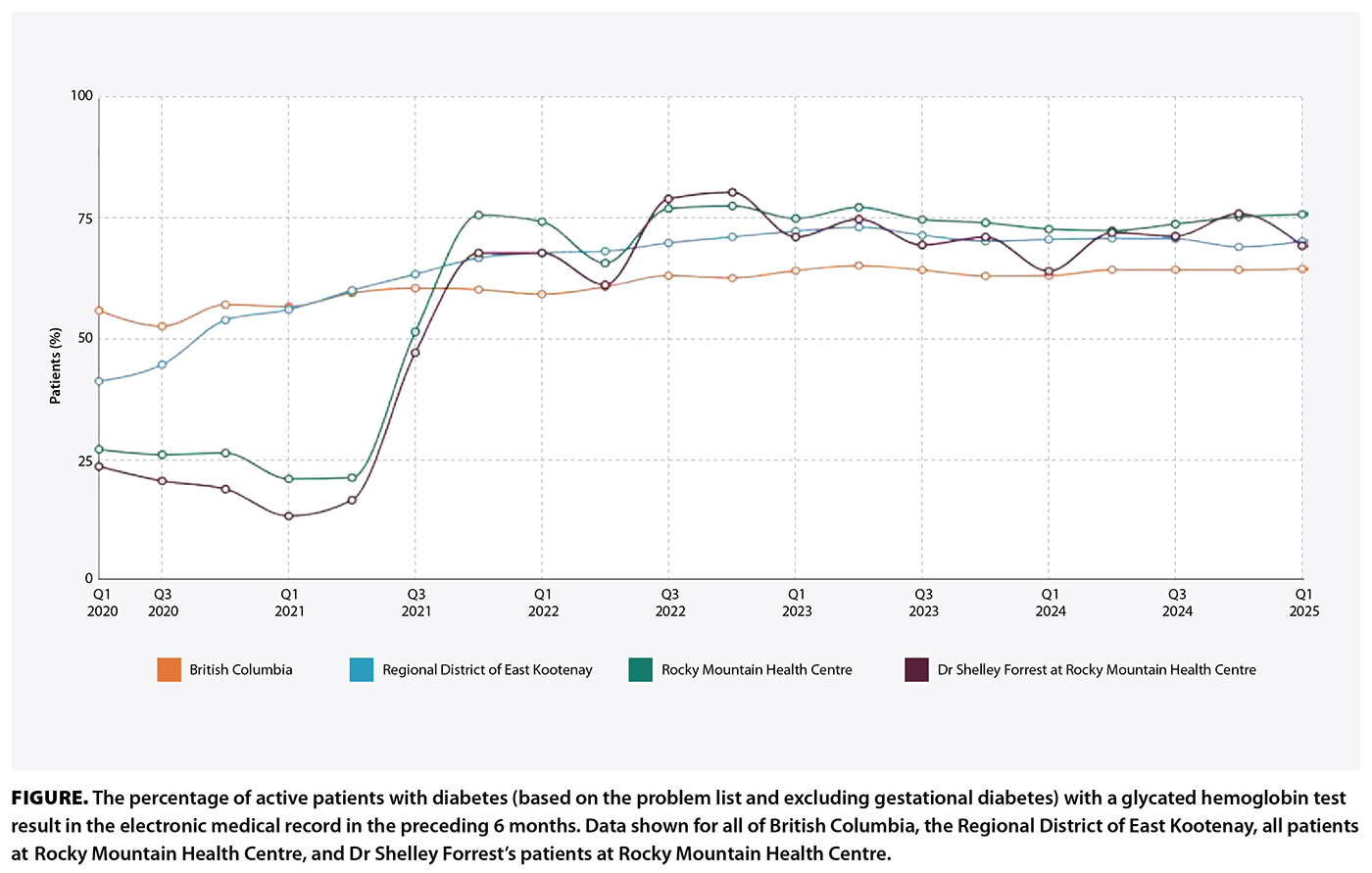 At Rocky Mountain Health Centre in Fernie, BC, six family physicians have contributed data to FPSC’s Health Data Coalition (HDC) since 2021. During the 18 months between Q1 2021 and Q3 2022, the percentage of diabetic patients who had a glycated hemoglobin test in the preceding 6 months increased from approximately 25% to approximately 75% [Figure]. These efforts have been well sustained over time, which is a tremendous feat.
At Rocky Mountain Health Centre in Fernie, BC, six family physicians have contributed data to FPSC’s Health Data Coalition (HDC) since 2021. During the 18 months between Q1 2021 and Q3 2022, the percentage of diabetic patients who had a glycated hemoglobin test in the preceding 6 months increased from approximately 25% to approximately 75% [Figure]. These efforts have been well sustained over time, which is a tremendous feat.
Dr Shelley Forrest says the significant improvement in diabetic care is directly correlated with their clinic acquiring a chronic disease team, particularly two chronic disease registered nurses, Lynn Walker and Leah Folkmann. Dr Forrest’s patients are supported and followed more comprehensively than a family physician can do alone.
The team usually sees a patient for the first 30 to 45 minutes of an appointment to conduct an in-depth assessment; then the physician joins them. Together, the team and the patient make a plan that includes diet, exercise, and medication recommendations. The patient receives foot care education; optometry and dental care recommendations; and information on how to recognize and treat hypoglycemia, how to plan for sick-day medication changes, and how to drive safely.
Results in the HDC Discover application clearly show that this 45-minute conversation between a registered nurse and the patient is time well spent.
How to advance your team-based approach
Initiating a team-based care model is a complex, multifaceted effort. In addition to practice supports provided by the PSP, FPSC offers team-based care grants of up to $15 000 to eligible family practices.[1] The grant helps with recruitment and onboarding costs, which are often a barrier to developing team-based practices.
High-functioning teams improve access and continuity by expanding clinical capacity, improving after-hours coverage, and extending the range and speed of accessing health services. Patients experience more timely care and greater satisfaction, while physicians realize a more sustainable practice model.
Learn more about how FPSC’s PSP team can optimize team-based care in your practice on the PSP (https://fpscbc.ca/psp) and Doctors Technology Office (www.doctorsofbc.ca/advice-support/doctors-technology-office) web pages, or submit a service request at www.doctorsofbc.ca/service.
HDC Discover helps physicians and clinics improve clinical practice, enhance patient care, and understand the impact of changes. Learn how FPSC’s HDC can help you plan and evaluate team-based care at https://hdcbc.ca.
—Jaron Easterbrook, MD
—Baldev Sanghera, MD
—Janet Evans, MD
—Greg Costello, MD
—Kevin Martin, MD
Family Practice Services Committee members
hidden
This article is the opinion of the authors and not necessarily the Family Practice Services Committee or Doctors of BC. This article has not been peer reviewed by the BCMJ Editorial Board.
 |
| This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. |
References
1. Family Practice Services Committee. Grant announced by GPSC to offset costs of recruiting into team-based care practices. Updated 13 May 2021. Accessed 2 June 2025. https://fpscbc.ca/news/news/grant-announced-gpsc-offset-costs-of-recruiting-team-based-care-practices.
