Clinical Images
Umbilical lesion: Granuloma or omphalomesenteric duct?
Sonographic, surgical, and histopathological findings may be required to distinguish between umbilical granulomas and polyps.
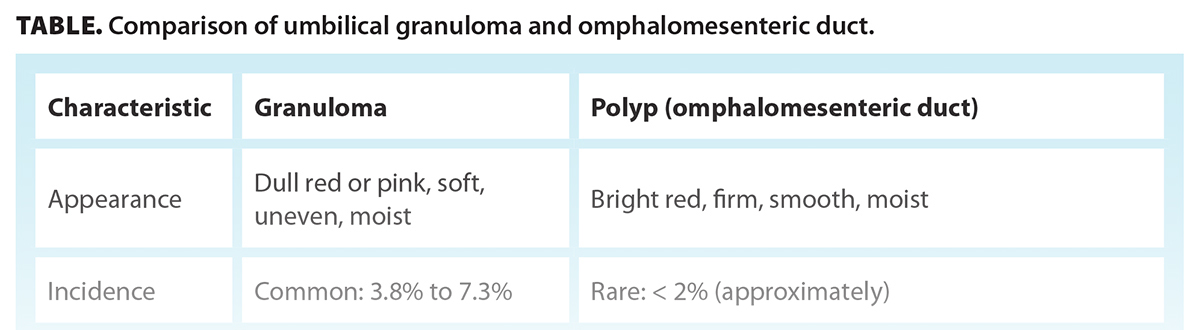
 An 11-month-old female presented with a firm, nontender, bright-red, moist umbilical lesion without obvious urine or bile discharge [Figure 1]. The child was otherwise well. The differential diagnosis included granuloma and omphalomesenteric duct remnant. However, the clinical manifestations were nonspecific, making differentiation difficult. Granulomas are common and are treated with topical silver nitrate; omphalomesenteric duct remnants are rare and require surgical excision [Table].
An 11-month-old female presented with a firm, nontender, bright-red, moist umbilical lesion without obvious urine or bile discharge [Figure 1]. The child was otherwise well. The differential diagnosis included granuloma and omphalomesenteric duct remnant. However, the clinical manifestations were nonspecific, making differentiation difficult. Granulomas are common and are treated with topical silver nitrate; omphalomesenteric duct remnants are rare and require surgical excision [Table].
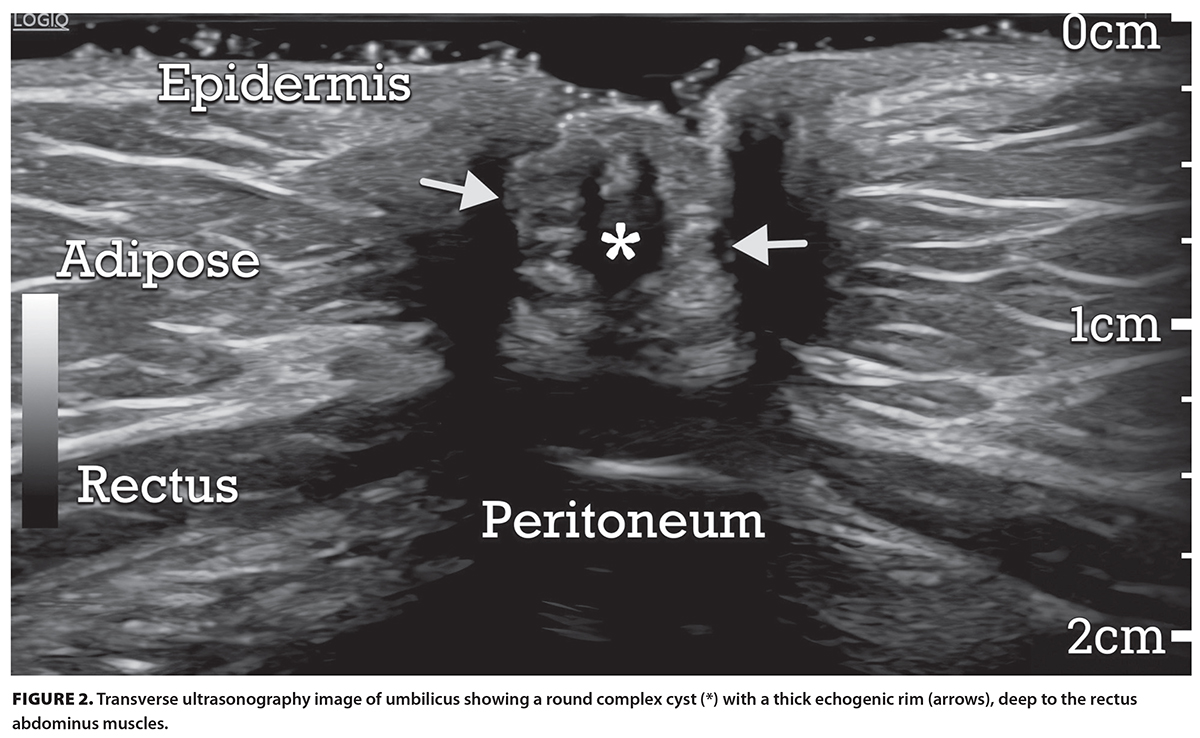
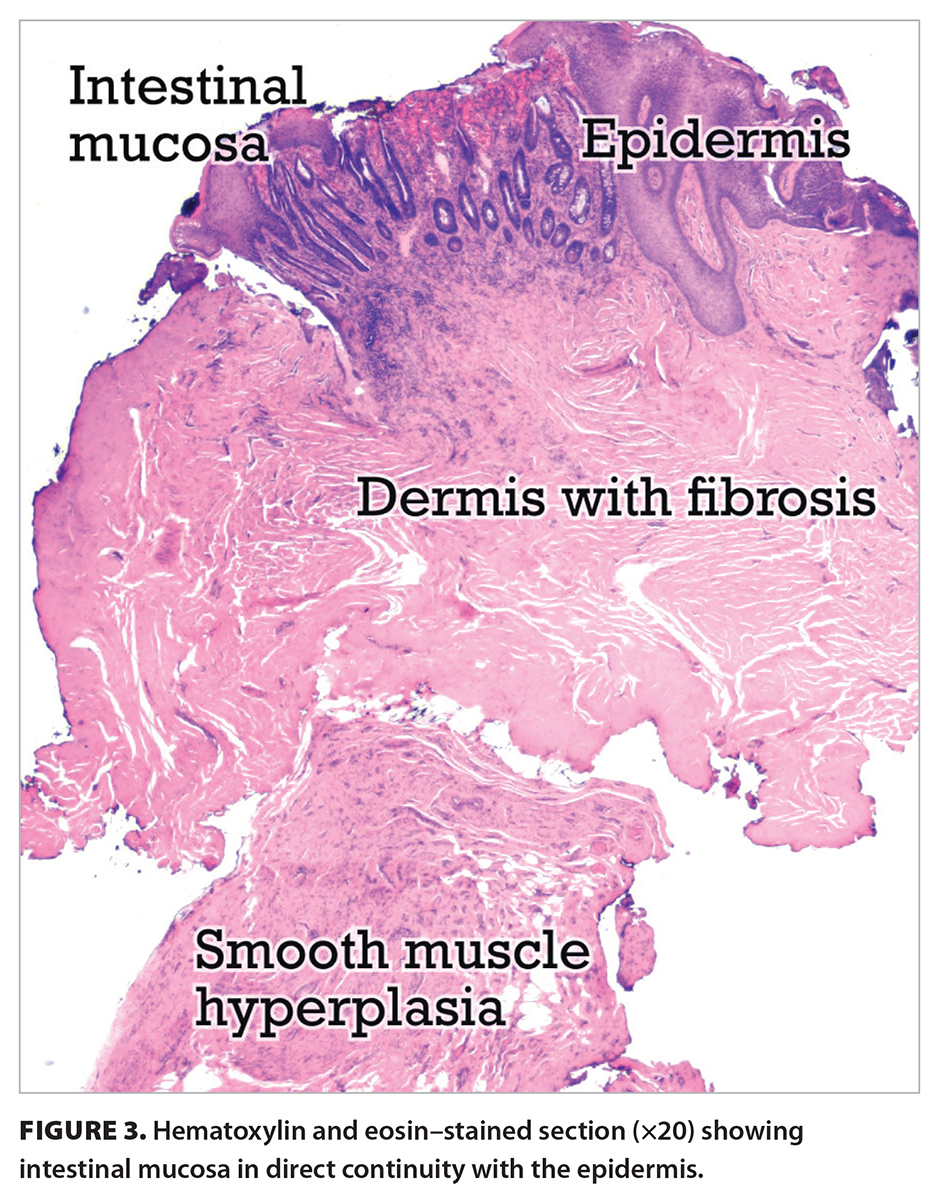
Initially, umbilical granuloma was suspected clinically and was treated with silver nitrate. When the lesion persisted, ultrasonography was performed, which revealed a deep-seated cyst inconsistent with a granuloma [Figure 2]. Given the uncertain diagnosis, the child was referred to pediatric surgery. At surgery, the lesion appeared similar to residual mucosa tissue but not patent to the internal organs. The sac was dissected from the base of the umbilicus and a cord-like structure that tapered off approximately 1 cm deep to the umbilical skin. Histologically, benign intestinal mucosa was seen in continuity with adjacent epidermis and both underlying dermal fibrosis and smooth muscle hyperplasia [Figure 3], which confirmed the diagnosis of omphalomesenteric duct remnant, specifically umbilical polyp.
 Disorders of the umbilicus in infancy are categorized as either abdominal wall defects, as in umbilical hernia, gastroschisis, and omphalocele; unobliterated embryological structures, as in urachal anomalies and omphalomesenteric remnant; or skin lesions, such as granulomas or dermoid cysts.
Disorders of the umbilicus in infancy are categorized as either abdominal wall defects, as in umbilical hernia, gastroschisis, and omphalocele; unobliterated embryological structures, as in urachal anomalies and omphalomesenteric remnant; or skin lesions, such as granulomas or dermoid cysts.
Approximately 2% of the population has an omphalomesenteric duct remnant, most commonly associated with an enteric Meckel diverticulum.[1-3] Sonographically, an umbilical polyp appears as a deep-seated cystic lesion with thick echogenic walls, with or without a sinus or deeper tract. The pathway for treatment typically begins with topical silver nitrate. Failure to respond is suggestive of an embryological defect. Ultrasonography may be helpful; however, final diagnosis usually requires histopathological examination.
Competing interests
None declared.
hidden
This article has been peer reviewed.
 |
| This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. |
References
1. Kim DH, Lee HJ, Kim JY, Jung HR. Differential diagnosis of umbilical polyps and granulomas in children: Sonographic and pathologic correlations. Ultrasonography 2021;40:248-255. https://doi.org/10.14366/usg.20020.
2. Bagade S, Khanna G. Imaging of omphalomesenteric duct remnants and related pathologies in children. Curr Probl Diagn Radiol 2015;44:246-255. https://doi.org/10.1067/j.cpradiol.2014.12.003.
3. Hsu JW, Tom WL. Omphalomesenteric duct remnants: Umbilical versus umbilical cord lesions. Pediatr Dermatol 2011;28:404-407.
hidden
Ms Letourneau is a sonographer in the Island Health Authority. Dr Gill is a dermatopathologist in the Island Health Authority and a clinical assistant professor in the Department of Pathology and Laboratory Medicine at the University of British Columbia. Mr Matsuo is a third-year kinesiology student at the University of Victoria. Dr Matsuo is a radiologist in the Island Health Authority.
Corresponding author: Ms Karen Letourneau, karenletourneau@me.com.