Youth suicide and self-harm by medications in BC: The role of means restriction
Means restriction is an evidence-based intervention that limits access to lethal means of suicide and serious self-harm. These interventions can form part of a comprehensive mental health and well-being strategy, which is particularly important given the recent decline in self-reported positive mental health and increase in self-harm indicators among youth in BC.[1]
Research indicates that greater availability of and access to lethal means of suicide and self-harm increase both population and individual risk of suicide, whereas restricting or limiting access decreases suicide rates, without evidence of suicide displacement (i.e., people considering suicide do not choose alternative means of self-harm as a result of means-restriction efforts).[2,3] Examples of means-restriction targets include firearms, jumping sites, and medications.
To inform suicide prevention efforts, a review was conducted of BC youth (10- to 24-year-olds) self-harm hospitalization data. Poisoning was identified as the leading cause of youth self-harm hospitalization, particularly among females [Table 1]. External causes of self-harm hospitalization (e.g., sharp objects, hanging, jumping) were significantly lower than poisoning. Although intentional poisoning contributes significantly to youth self-harm hospitalization in BC, it is not a top cause of death by suicide.
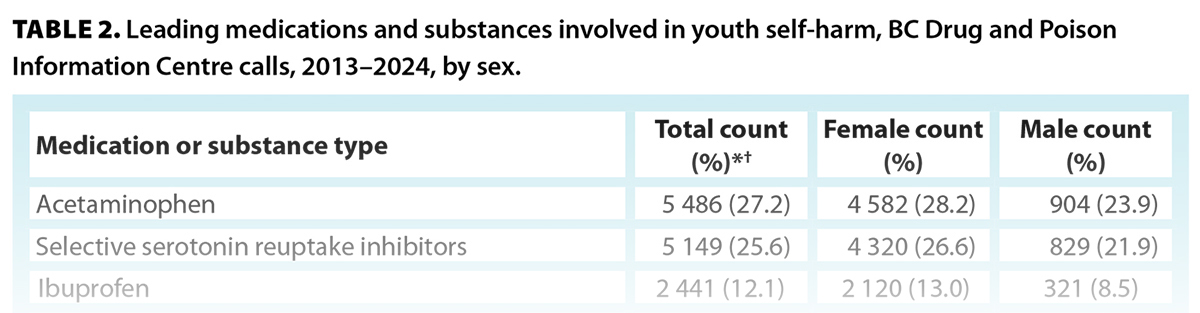
A review of BC Drug and Poison Information Centre data identified the most common substances involved in youth self-harm calls [Table 2]. The leading classes/types of medications in the calls about youth self-harm were acetaminophen, selective serotonin reuptake inhibitors, ibuprofen, and antipsychotics. This is likely because of their relative availability to youth. Antidepressants, mood stabilizers, and anti-anxiety medications are commonly prescribed to youth for the management of depression and anxiety and were commonly involved in self-harm calls. Youth who are at greater risk of suicide and self-harm are more likely to have access to these medications than the public. Several of the top culprit medications, such as acetaminophen, ibuprofen, and diphenhydramine, are available over the counter and can be accessed in large quantities by the Canadian public.
These findings highlight opportunities for prescribers, policymakers, and the public to reduce the risk of youth self-harm and suicide. Potential actions include incorporating safety considerations into prescribing guidelines, modifying prescribing practices for higher-risk patients, and providing education to patients and families on safe medication storage and disposal. Means-prevention interventions for over-the-counter medications in other jurisdictions can inform local approaches. For example, the United Kingdom introduced legislation in 1998 to limit over-the-counter acetaminophen package sizes, resulting in a 43% reduction in suicide deaths due to acetaminophen over 11 years.[4]
Limiting access to a lethal supply of medications is an evidence-based approach to prevention of youth suicide and self-harm. Greater awareness of the epidemiology of medication self-harm can inform strategies to reduce youth self-harm.
—Brandon Yau, MD, MPH, CCFP, FRCPC
Medical Health Officer, Vancouver Coastal Health
—Mojgan Karbakhsh, MD, MPH
Researcher, BC Injury Research and Prevention Unit, BC Children’s Hospital Research Institute
—Megan Oakey, MPH
Manager, Injury Prevention, BCCDC
—Jeffrey Trieu, MPH
Senior Epidemiologist, Environmental Health Services, BCCDC
hidden
This article is the opinion of the BC Centre for Disease Control and has not been peer reviewed by the BCMJ Editorial Board.
 |
| This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. |
References
1. Smith A, Poon C, Peled M, et al. The big picture: An overview of the 2023 BC Adolescent Health Survey provincial results. Vancouver, BC: McCreary Centre Society; 2024. https://doi.org/10.13140/RG.2.2.33402.88008.
2. Hawton K, Knipe D, Pirkis J. Restriction of access to means used for suicide. Lancet Public Health 2024;9:E796-E801. https://doi.org/10.1016/S2468-2667(24)00157-9.
3. Lim JS, Buckley NA, Chitty KM, et al. Association between means restriction of poison and method-specific suicide rates: A systematic review. JAMA Health Forum 2021;2:e213042. https://doi.org/10.1001/jamahealthforum.2021.3042.
4. Hawton K, Bergen H, Simkin S, et al. Long term effect of reduced pack sizes of paracetamol on poisoning deaths and liver transplant activity in England and Wales: Interrupted time series analyses. BMJ 2013;346:f403. https://doi.org/10.1136/bmj.f403.



thanks for info.