The role of mitochondria in aging, neurodegenerative disease, and future therapeutic options
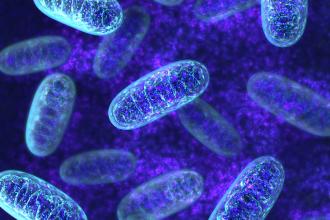
ABSTRACT: The mitochondrion is an essential organelle central to a number of biochemical processes in the cell. Since we know the functional efficiency of mitochondria declines with age, and since aging is a risk factor common to a number of neurodegenerative diseases, including Alzheimer disease, Parkinson disease, and amyotrophic lateral sclerosis, researchers have proposed that secondary mitochondrial failure may be the common pathway in-volved in degenerative processes. Given the evidence suggesting that mitochondrial dysfunction and oxidative damage play a role in neurodegeneration, researchers are looking at antioxidant therapies. Although there is no evidence supporting the use of common over-the-counter antioxidants such as vitamins C and E in the treatment or prevention of neurodegenerative diseases, other therapeutic agents aimed at restoring or preserving mitochondrial health hold promise for treating these diseases in the future.
Therapies based on agents that enhance mitochondrial health may eventually play a role in the treatment of Alzheimer disease and other neurodegenerative conditions.
Aging is natural to all of us, and can be defined as a time-dependent degenerative process that ultimately leads to death. The idea that free radicals and oxidative damage might lead to aging and premature cell death has been around since our early understanding of the biochemistry involved in energy production in organisms.
Harman first suggested that oxidative damage to cellular components produced by free radicals is the underlying cause of aging, based on the observation that ionizing radiation and oxygen pressures decrease life span.[1]
He later specified that oxidative damage to mitochondria is the determining factor, and suggested that mitochondria might be the “biological clock” that governs longevity.[2]
A number of observations have led researchers to speculate that mitochondrial dysfunction may be a common denominator in neurodegenerative processes that ultimately lead to cell death. First, the most important risk factor common to neurodegenerative diseases such as Alzheimer disease (AD), Parkinson disease (PD), and amyotrophic lateral sclerosis (ALS) is aging, and we know mitochondrial efficiency declines with age.
Second, many mitochondrial proteins possess iron-sulfur clusters for oxidation-reduction reactions and are constantly under the threat of oxidative damage.
Third, unpaired electrons generated in binding sites of complex I, II, and III of the electron transport chain can produce superoxide radicals, which do not easily pass though biological membranes and thus must be inactivated within the mitochondrion itself, causing local damage.
Fourth, mitochondrial DNA (mtDNA) lacks protective histones, and is particularly vulnerable to the attack of reactive oxygen species (ROS), leading to long-term damage of the organelle.[3] These aspects of mitochondrial function have led researchers to hypothesize that antioxidants may be helpful in managing neurodegenerative disorders (Table).
Alzheimer disease
Alzheimer disease is the most common cause of dementia, and is also the most common neurodegenerative disease in humans. It is characterized by progressive decline in memory and other cognitive functions.
The neuropathological hallmarks of AD include senile plaques formed by the aggregation of beta amyloid (Ab) peptides, and neurofibrillary tangles made up mainly of tau protein from microtubules in neurons. The development of plaques and tangles is followed by loss of synapses, depletion of neurotransmitters, and, ultimately, neuronal cell death and cerebral atrophy.
Exactly how Ab causes brain cell death continues to be an area of intense research. A number of recent studies have demonstrated a connection between mitochondrial dysfunction and AD. Defective glucose utilization is an early event in AD, suggesting possible abnormalities in mitochondrial function.
It has also been shown that Ab can generate free radicals in vitro, which can directly disrupt mitochondrial function by inhibiting several key enzymes in the mitochondrial energy production pathway.[4] In addition, cytochrome c oxidase activity is reduced in postmortem brain tissue of AD patients.[5]
Moreover, animal models of AD have demonstrated that mitochondrial impairment can lead to disruption of calcium homeostasis in the neuron, further implicating mitochondrial dysfunction in the pathogenesis of AD.[6]
Another way mitochondria may be involved in the pathogenesis of AD is through apoptosis, or programmed cell death. A number of studies suggest that Ab can induce apoptosis in neurons directly, and increase their vulnerability to cell death by increasing oxidative stress and reducing energy availability.[7]
Beta amyloid can also inhibit alcohol dehydrogenase activity, which in turn leads to upstream accumulation of toxic metabolites, and ultimately causes leakage of mitochondrial oxygen free radicals and impaired cellular energy production.[8]
Some recent studies have also found that excessive tau, the major component of neurofibrillary tangles in AD brains, can also lead to mitochondrial dysfunction. NADH-CoQ oxidoreductase (complex I) activity is reduced in transgenic mice overexpressing tau.[9]
Taken together, these findings suggest mitochondria play an important role, directly or indirectly, in the pathogenesis of AD, and treatment that preserves mitochondrial function and integrity may extend the remaining neuronal life in patients with AD.
Parkinson disease
Parkinson disease is a common movement disorder and the second most common neurodegenerative disease. Prevalence rates of 1% in the 60-plus age group and 4% among those 80 and over suggest that aging is an important risk factor.[10]
The diagnosis of PD is typically based on the clinical signs of resting tremor, bradykinesia, rigidity, and postural instability. Various nonmotor features may also develop, such as autonomic dysfunction, cognitive impairment, and sleep disturbances, suggesting a more widespread process of neurodegeneration.
PD is characterized by loss of dopaminergic neurons in the substantia nigra leading to dopamine deficiency in the striatum. The pathological hallmark of PD is the presence of Lewy bodies, protein deposits composed mainly of a-synuclein, within neurons in the substantia nigra. The cause of PD is unknown, but like AD, it is a complex multifactorial disorder likely to be associated with environmental risk factors and genetic susceptibility.
In the 1970s, a parkinsonian syndrome was observed in number of intravenous drug users. Subsequently, the causative agent was found to be MPTP, a contaminant in the illegal production of meperidine, a narcotic related to heroin.[11]
The autopsy of a patient with MPTP-induced parkinsonism revealed dopaminergic neuronal loss in the substantia nigra as in idiopathic PD, although Lewy bodies were not seen. Animal studies later demonstrated that within neurons a toxic metabolite of MPTP is generated in mitochondria and inhibits normal electron transport, resulting in decreased adenosine triphosphate (ATP) production and increased generation of ROS.
A number of subsequent studies confirmed that the toxic metabolite inhibits complex I activity and induces proteasomal deregulation, and in turn exacerbates protein aggregation and ultimate demise of the substantia nigral dopaminergic neurons.[12]
In addition to studies describing the role of MPTP in neurodegeneration, epidemiological studies have linked pesticide exposure to higher risk of developing PD. In particular, rotenone, a naturally occurring common pesticide, is a highly potent inhibitor of complex I, and many of the features of PD associated with degeneration of dopaminergic neurons have been reproduced in rat models.[13]
Recent genetic studies also suggest that mitochondrial dysfunction may play a central role in the pathogenesis of PD. For instance, the parkin gene mutations account for the majority of autosomal recessive PD.[14]
Parkin protects neurons against a wide spectrum of stressors, including excitotoxicity, mitochondrial dysfunction, and overexpression of a-synuclein. A more recent large-scale genome-wide meta-analysis found a number of gene sets associated with PD, suggesting that defects in mitochondrial electron transport and glucose metabolism are involved.[15]
Amyotrophic lateral sclerosis
After AD and PD, amyotrophic lateral sclerosis is the third most common adult-onset neurodegenerative disease in humans. It is a progressive, severely debilitating disease characterized by muscle weakness, muscle atrophy, spasticity, and eventual paralysis and death, typically within 3 to 5 years of symptom onset. It is still not clear why the anterior horn cells of the spinal cord and cortical motor neurons are selectively vulnerable in ALS.
While previously felt to be mostly a “pure motor” disease, ALS is now recognized to affect frontal lobe executive function as well in a significant proportion of patients, with 5% having an overt frontotemporal dementia.[16] Other than age, the only indisputable risk factor for ALS is genetic susceptibility, with familial cases occurring in about 10% of most case series.
The first gene identified for familial ALS is the copper-zinc superoxide dismutase 1 (SOD1), responsible for 15% to 20% of all familial ALS cases. SOD1 is an endogenous free radical scavenger that detoxifies and maintains intracellular concentration of the reactive superoxide radical at low level by catalyzing its dismutation.
SOD1 is ubiquitous in most tissues, with possibly the highest levels within neurons. Expression of mutant SOD1 in cell culture results in abnormal mitochondria with decreased activities of complex II and IV of the electron transport chain. In addition, motor neurons expressing mutant SOD1 show accelerated cell death when exposed to oxidative stress.[17]
Mitochondrial vaculolization has been observed as an early pathological feature before neuronal death in transgenic mice with mutant SOD1. In addition, elevated calcium levels can prevent anterograde axonal transport by preventing proper kinesin binding to microtubules.[18]
Furthermore, aggregation of mutant SOD1 along microtubules may interfere with both anterograde and retrograde transport by acting like a blockade. Other mitochondrial changes associated with ALS include diminished levels or multiple deletions of mtDNA in skeletal muscle biopsies of ALS patients.
Other neurodegenerative diseases
In addition to AD, PD, and ALS, other neurodegenerative diseases have been linked to secondary mitochondrial dysfunction in their pathogenesis. Friedreich ataxia is the most common neurodegenerative genetic progressive ataxia with autosomal recessive inheritance. The mutation occurs in a protein called frataxin, which is now known to be essential for mitochondrial oxidative phosphorylation and iron homeostasis.[19]
The genetic defect impairs incorporation of iron into iron-sulfur clusters, which leads to iron accumulation in mitochondria and subsequent impairment of activities involving enzymes containing iron-sulfur in complex I and II of the electron transport chain.
Huntington’s disease (HD) is an autosomal dominant neurodegenerative disease characterized by chorea and cognitive impairment. Biochemical studies showing reduction in complex II, complex III, and aconitase activity in the basal ganglia of HD patients suggest mitochondrial dysfunction may play an important role.[20] Furthermore, systemic administration of mitochondrial toxin reproduces HD pathology in animals.
Antioxidant therapy
Given the evidence indicating that mitochondrial dysfunction plays a role in neurodegeneration, therapeutic approaches targeting mitochondrial dysfunction and oxidative damage in neurodegenerative diseases look promising.
A number of antioxidants, including beta carotene and vitamins C and E, have been examined. Several bioenergetic therapies believed to improve mitochondrial function, including therapies based on creatine, coenzyme Q10 (CoQ), idebenone, and calorie-restricted diets are being tested for their neuroprotective efficacy in these disorders.
Vitamin E, or a-tocopherol, is a fat-soluble antioxidant that stops the production of ROS when fat undergoes oxidation. Preclinical studies in animals and cell models have found that oral supplementation of vitamin C (ascorbic acid) and vitamin E alone and in combination decrease oxidative DNA damage.
Unfortunately, systematic reviews of observational studies have not found any consistent benefit with vitamin C or beta carotene in AD or PD, and evidence in ALS is lacking.[21] Only vitamin E has been examined in randomized clinical trials for use in AD, but to date there is no conclusive evidence suggesting any significant benefits in symptomatic treatment or prevention of progression in AD.[22]
Creatine, a naturally occurring nitrogenous organic acid, has shown promising neuroprotective effects in animals and is being studied for treating PD, HD, and ALS. CoQ is a lipid-soluble endogenous compound that serves as a cofactor for the electron transport chain by accepting electrons from complex I, II, and III. It serves as a potent free radical scavenger in the mitochondria.
Clinical trials of CoQ as a treatment option for PD are underway based on promising results in pilot studies. A synthetic analog of CoQ, idebenone, was found to protect neurons from beta-amyloid-induced toxicity in preclinical studies, but the results in a large-scale AD treatment trial were negative.[23]
Idebenone looks more promising for the treatment of Friedreich ataxia, especially in younger patients, and phase 3 clinical trials are underway. The calorie-restricted diet is emerging as another novel way to affect mitochondrial function, with mice on calorie-restricted diets showing diminished Ab production and reduced amyloid plaque deposition.
The efficacy of these and other therapies designed to enhance mitochondrial function will be known when results of ongoing clinical studies become available.
Conclusions
There is mounting evidence that secondary mitochondrial dysfunction occurs in a number of major neurodegenerative diseases, including Alzheimer disease, Parkinson disease, amyotrophic lateral sclerosis, Huntington disease, and Friedreich ataxia.
As these diseases bring devastation and despair to the patient and family, even small improvements in symptoms can be of significant clinical benefit. In the future, well-designed and well-executed clinical trials will provide more definitive information on the therapeutic efficacy of agents aimed at improving mitochondrial health.
As research in the metabolic field advances, we can look forward to improved understanding and better interventions for these debilitating diseases.
Acknowledgments
Dr Hameed has received the Higher Manpower Development award from SingHealth, Singapore, for his fellowship in dementia.
Dr Hsiung is supported by a Clinical Genetics Investigatorship award from the Canadian Institute of Health Research, and the Fisher Professorship from the Alzheimer Society of British Columbia.
Competing interests
None declared.
References
1. Harman D. Aging: A theory based on free radical and radiation chemistry. J Gerontol 1956;11:298-300.
2. Harman D. The biologic clock: The mitochondria? J Am Geriatr Soc 1972;20:145-147.
3. Wallace DC. A mitochondrial paradigm of metabolic and degenerative diseases, aging, and cancer: A dawn for evolutionary medicine. Annu Rev Genet 2005;39:359-407. PubMed Abstract.
4. Keil U, Bonert A, Marques CA, et al. Amyloid beta-induced changes in nitric oxide production and mitochondrial activity lead to apoptosis. J Biol Chem 2004;279:50310-50320. PubMed Abstract.
5. Kish SJ, Bergeron C, Rajput A, et al. Brain cytochrome oxidase in Alzheimer’s disease. J Neurochem 1992;59:776-779. PubMed Abstract.
6. Mancuso M, Siciliano G, Filosto M, et al. Mitochondrial dysfunction and Alzheimer’s disease: New developments. J Alzheimers Dis 2006;9:111-117. PubMed Abstract.
7. Sultana R, Butterfield DA. Alterations of some membrane transport proteins in Alzheimer’s disease: Role of amyloid beta-peptide. Mol Biosyst 2008;4:36-41. PubMed Abstract.
8. Takuma K, Yao J, Huang J, et al. ABAD enhances Abeta-induced cell stress via mitochondrial dysfunction. FASEB J 2005;19:597-598. PubMed Abstract.
9. David DC, Hauptmann S, Scherping I, et al. Proteomic and functional analyses reveal a mitochondrial dysfunction in P301L tau transgenic mice. J Biol Chem 2005;280:23802-23814. PubMed Abstract.
10. de Lau LM, Breteler MM. Epidemiology of Parkinson’s disease. Lancet Neurol 2006;5:525-535. PubMed Abstract.
11. Langston JW, Ballard P, Tetrud JW, et al. Chronic parkinsonism in humans due to a product of meperidine-analog synthesis. Science 1983;219:979-980. PubMed Abstract.
12. Schapira AH, Cooper JM, Dexter D, et al. Mitochondrial complex I deficiency in Parkinson’s disease. J Neurochem 1990;54:823-827. PubMed Abstract.
13. Gomez C, Bandez MJ, Navarro A. Pesticides and impairment of mitochondrial function in relation with the parkinsonian syndrome. Front Biosci 2007;12:1079-1093. PubMed Abstract.
14. Farrer MJ. Genetics of Parkinson disease: Paradigm shifts and future prospects. Nat Rev Genet 2006;7:306-318. PubMed Abstract.
15. Zheng B, Liao Z, Locascio JJ, et al.; Global PD Gene Expression (GPEX) Consortium. PGC-1, a potential therapeutic target for early intervention in Parkinson’s disease. Sci Transl Med 2010;2:52ra73.
16. Mackenzie IR, Feldman HH. Ubiquitin immunohistochemistry suggests classic motor neuron disease, motor neuron disease with dementia, and frontotemporal dementia of the motor neuron disease type represent a clinicopathologic spectrum. J Neuropathol Exp Neurol 2005;64:730-739. PubMed Abstract.
17. Menzies FM, Cookson MR, Taylor RW, et al. Mitochondrial dysfunction in a cell culture model of familial amyotrophic lateral sclerosis. Brain 2002;125(Pt 7):1522-1533. PubMed Abstract.
18. Tortarolo M, Veglianese P, Calvaresi N, et al. Persistent activation of p38 mitogen-activated protein kinase in a mouse model of familial amyotrophic lateral sclerosis correlates with disease progression. Mol Cell Neurosci 2003;23:180-192. PubMed Abstract.
19. Lynch DR, Farmer JM, Balcer LJ, et al. Friedreich ataxia: Effects of genetic understanding on clinical evaluation and therapy. Arch Neurol 2002;59:743-747. PubMed Abstract.
20. Browne SE, Beal MF. The energetics of Huntington’s disease. Neurochem Res 2004;29:531-546. PubMed Abstract.
21. Etminan M, Gill SS, Samii A. Intake of vitamin E, vitamin C, and carotenoids and the risk of Parkinson’s disease: A meta-analysis. Lancet Neurol 2005;4:362-365. PubMed Abstract.
22. Isaac MG, Quinn R, Tabet N. Vitamin E for Alzheimer’s disease and mild cognitive impairment. Cochrane Database Syst Rev 2008(3):CD002854.
23. Thal LJ, Grundman M, Berg J, et al. Idebenone treatment fails to slow cognitive decline in Alzheimer’s disease. Neurology 2003;61:1498-1502. PubMed Abstract.


I am inquiring about obtaining a copy of an article titled, "The role of mitochondria in aging, neurodegenerative disease, and future therapeutic options" at: https://bcmj.org/articles/role-mitochondria-aging-neurodegenerative-dise... for a friend that has Chorea. I can only print out the first page.
Would it be possible?
Thank you.