Original Research
Climate impact of inhaler therapy in the Fraser Health region, 2016–2021
ABSTRACT
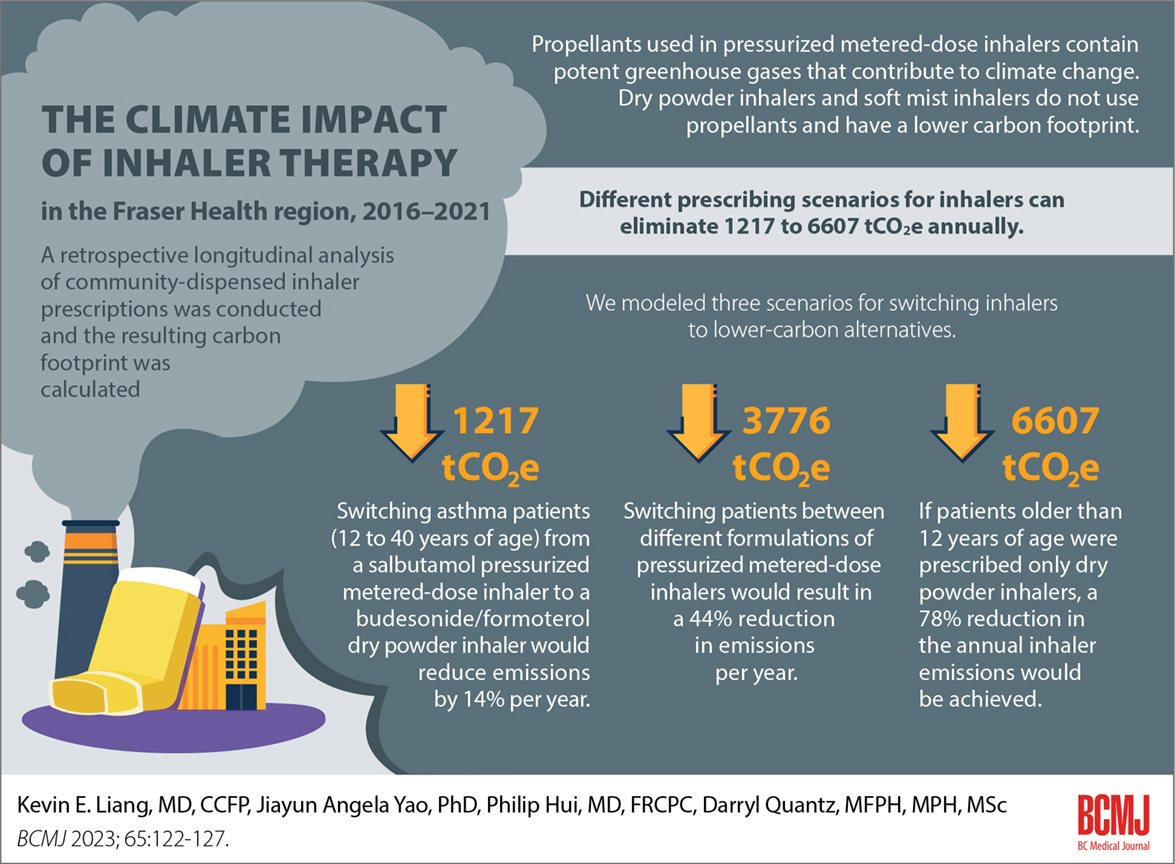
Background: Inhaler therapy is a cornerstone treatment for asthma and chronic obstructive pulmonary disease. Propellants used in pressurized metered-dose inhalers contain potent greenhouse gases that contribute to climate change. Dry powder inhalers and soft mist inhalers do not use propellants and have a lower carbon footprint.
Methods: We conducted a retrospective longitudinal analysis of community-dispensed inhaler prescriptions in the Fraser Health region in British Columbia from 2016 to 2021 and calculated the resulting carbon footprint. We modeled three scenarios for switching inhalers to lower-carbon alternatives.
Results: The average annual carbon footprint of inhalers was 8478 tonnes of CO2 equivalent (tCO2e), which was 21.8% of the reported total emissions from Fraser Health facilities. Different prescribing scenarios for inhalers can eliminate 1217 to 6607 tCO2e annually.
Conclusions: Encouraging switches to low-carbon inhalers offers an opportunity to reduce health care–associated carbon emissions and potentially improve respiratory care.
Switching away from pressurized metered-dose inhalers with high carbon footprints, when appropriate, would reduce the health care sector’s greenhouse gas emissions and could improve respiratory care.
Background
Health care–related carbon emission is a significant contributor to climate change; it is estimated to constitute 4.6% of the global carbon footprint.[1] When compared with the health care systems of 47 countries, the carbon footprint of the Canadian health care system is the third highest in the world on a per capita basis.[2,3]
A group of medications called pressurized metered-dose inhalers, which are used for managing obstructive lung diseases such as asthma and chronic obstructive pulmonary disease, have an outsized carbon footprint. Because pressurized metered-dose inhalers use liquefied gases called hydrofluoroalkanes (HFAs) as propellants to deliver medication to the lungs, they release potent greenhouse gases into the atmosphere on actuation and if disposed of improperly.[4] Pressurized metered-dose inhalers account for 70% of inhalers prescribed in the United Kingdom and up to 4% of its health care carbon footprint.[5,6]
Low-carbon alternatives to pressurized metered-dose inhalers are readily available in Canada. HFA-free dry powder inhaler and soft mist inhaler formulations have similar effects as those of pressurized metered-dose inhalers but with reduced climate impact.[7]
In this study, we reviewed the prescribing patterns for and calculated the climate impact of inhalers available in the Fraser Health region. Fraser Health is the most populous health region in British Columbia; it includes 20 communities from Burnaby to the Fraser Canyon and has an estimated population of 1.9 million.[8] We also estimated the prevalence of overuse of short-acting ß2-agonists, which results in significant greenhouse gas emissions and can be used independently to predict adverse respiratory health outcomes.[9] Finally, we modeled three scenarios for reducing emissions with altered inhaler prescription patterns and discuss their indirect potential to improve respiratory care.
Methods
Ethics review and approval for this study were waived by the Fraser Health Research Ethics Board.
Data sources
PharmaNet
All prescriptions dispensed in community pharmacies in BC are recorded in the PharmaNet system. We requested PharmaNet data for Fraser Health region residents from 1 January 2016 to 31 December 2021 via the Health Data Platform BC.[10] Dispensed inhalers were identified and categorized into pressurized metered-dose inhalers or dry powder inhalers/soft mist inhalers by their drug identification number. Information on the date the inhaler was dispensed and the age of the individual who received the inhaler was obtained. Unique study subject identifications were also used.
Inhaler carbon footprint
We used the Health Canada Drug Product Database to determine the availability of inhalers in Canada and obtain their drug identification numbers. To calculate the carbon footprint of every inhaler available in the Fraser Health region, we took the following steps:
- We used the manufacturer’s footprint values that were certified by the Carbon Trust—a global organization that verifies the carbon footprint data supplied by various companies.[7]
- When no manufacturer data were provided, we used values from PrescQIPP—a UK organization that generates carbon footprint data through a survey sent to pharmaceutical companies.[11] We ensured that the inhalers available in BC matched the dose, brand, ingredients, and mechanism of administration of the equivalent UK products.
- For the remaining inhalers, we followed PrescQIPP’s methods and estimated the carbon footprint of pressurized metered-dose inhalers by multiplying the inhaler’s propellant weight by the propellant’s global warming potential.
Fraser Health carbon footprint
Each year, Fraser Health releases its Climate Change Accountability Report, which summarizes the health authority’s measured carbon footprint, including buildings (fuel combustion and electricity), mobile fleet combustion, and paper.[12] The total footprint excludes any prescription data. We obtained the annual total emissions from Fraser Health for 2016 to 2021.
Data analyses
Data cleaning, analysis, and visualization were conducted using R (Version 4.1.3) on the Health Data Platform BC secure virtual desktop environment.
Overuse of short-acting ß2-agonists
We defined the rate of short-acting ß2-agonists overuse as the number of individuals 12 to 40 years of age who were dispensed three or more short-acting ß2-agonist inhalers in a calendar year, divided by the number of individuals 12 to 40 years of age who received at least one inhaler in the same year. This definition approximates the definition of overuse in the Global Initiative for Asthma guideline.[9,13,14]
Scenario development
Three scenarios were developed to calculate the potential reduction in greenhouse gas emissions due to altered patterns of inhaler use. In the first scenario, we replaced each pressurized metered-dose inhaler that contained higher volumes of propellants with pressurized metered-dose inhalers that offered the same or similar medication but contained lower volumes of propellant. Teva-Salbutamol and Airomir deliver the same medication as all other salbutamol pressurized metered-dose inhaler preparations (i.e., Ventolin) but have a reduced amount of propellant and thus a lower carbon footprint.[11] In addition, Zenhale, a pressurized metered-dose inhaler that is available in BC, uses a type of propellant that has a much higher global warming potential (HFA-227) than all other available pressurized metered-dose inhalers (HFA-134a).[11] In the second scenario, we replaced pressurized metered-dose inhalers prescribed to patients 12 years of age and older with the available equivalent dry powder inhaler formulation that offered the same or similar medication at equivalent doses. In the third scenario, we followed the current evidence-based asthma guideline, which calls for patients who are 12 years of age and older and have mild and very mild asthma to use budesonide-formoterol (a dry powder inhaler) solely instead of the pressurized metered-dose inhaler short-acting ß2-agonists as a rescue inhaler.[13,14] We restricted this replacement to those between 12 and 40 years of age to prevent the inclusion of older patients with chronic obstructive pulmonary disease. The supplementary data (available online) list the inhaler switches undertaken in each scenario. Inhalers contain varying doses depending on the device type and medication. We used a dose-to-dose substitution to model inhaler switches and to calculate the carbon footprint reduction.
Results
From 2016 to 2021, 70 unique inhaler devices were commonly available in the Fraser Health region, primarily for treatment of asthma and chronic obstructive pulmonary disease: 20 were pressurized metered-dose inhalers, 47 were dry powder inhalers, and 3 were soft mist inhalers. In the Fraser Health region between 2016 to 2021, the carbon footprint of available pressurized metered-dose inhalers ranged from 9720 to 36 500 gCO2e (grams of carbon dioxide equivalent) per inhaler; the range for dry powder inhalers/soft mist inhalers is 282 to 1700 gCO2e per inhaler.
From 2016 to 2021, more than 3.56 million inhalers were prescribed for Fraser Health region residents; an average of 394 094 pressurized metered-dose inhalers and 199 536 dry powder inhalers/soft mist inhalers were dispensed per year [Table 1]. The resulting carbon footprint of inhalers was 8478 tCO2e per year, and pressurized metered-dose inhalers accounted for more than 98% of the footprint [Figure 1]. To put this in context, the annual average measured emissions from the Fraser Health region, which includes 174 buildings with 13 acute care hospitals in 2021, over the same 6-year period was 38 951 tCO2e.[12]
Approximately 4.1% of patients between 0 and 9 years of age were prescribed at least one dry powder inhaler/soft mist inhaler. The proportion for patients 50 years of age and older increased to 41%, which illustrates a trend toward nonpressurized metered-dose inhaler use in older age groups. An average of 12.9% of patients between 12 and 40 years of age were prescribed three or more short-acting ß2-agonist inhalers per year during the 6-year period [Table 2].
The three scenarios for altered inhaler prescribing patterns resulted in significant emission reduction [Figure 2]:
- Switching patients between different formulations of pressurized metered-dose inhalers would result in a reduction in emissions of 3776 tCO2e (44%) per year.
- If patients older than 12 years of age were prescribed only dry powder inhalers, a reduction in emissions of 6607 tCO2e per year, or 78% of annual inhaler emissions, would be achieved.
- Switching asthma patients who are between 12 and 40 years of age from a salbutamol pressurized metered-dose inhaler to a budesonide/formoterol dry powder inhaler would reduce emissions by 1217 tCO2e (14%) per year.
Discussion
To our knowledge, this is the first study that has evaluated the climate impact of inhaler therapy in Canada based on prescription data. Our results show that pressurized metered-dose inhalers alone release approximately one-fifth of the emissions produced by Fraser Health facilities. Patients were prescribed a far greater proportion of pressurized metered-dose inhalers than lower-carbon alternatives that have similar expected efficacy. A method of reducing the inhaler footprint involves switching patients to a dry powder inhaler when clinically appropriate, which mirrors prescribing patterns used in Sweden, where only 13% of inhalers prescribed are pressurized metered-dose inhalers.[5]
In addition to their outsized climate impact, pressurized metered-dose inhalers present various clinical concerns. Suboptimal inhaler technique is common with pressurized metered-dose inhalers used in the outpatient setting.[15] Dry powder inhalers and soft mist inhalers, if used appropriately, can lead to greater medication deposition on the airways compared with pressurized metered-dose inhalers.[16] In addition, due to a lack of dose counter on many pressurized metered-dose inhalers, patients often have trouble determining when their pressurized metered-dose inhalers are empty, which results in either inappropriate disposal of nonempty inhalers or, conversely, the continued use of empty inhalers.[17] Finally, many dry powder inhalers and soft mist inhalers offer once-a-day dosing, which can reduce the respiratory “pill burden” and improve adherence.
Among all pressurized metered-dose inhalers, salbutamol remains the single largest source of carbon emissions from the Fraser Health region: it generates 5640 tCO2e per year, or 67% of the total inhaler footprint. Many patients with asthma are commonly prescribed salbutamol or short-acting ß2-agonists-only treatment, but frequent, single-agent salbutamol use is associated with poor asthma control and increased exacerbations, hospitalization, and death.[9] In our analysis, an annual average of 12.9% of patients between 12 and 40 years of age in the Fraser Health region are prescribed three or more short-acting ß2-agonist inhalers each year, an independent risk factor for asthma exacerbations leading to increased mortality and morbidity.[13,14]
Although efforts are made to reduce the greenhouse gas emissions associated with inhalers, patient choice should be central to decision-making; changes ought to be made only when clinically advantageous. Children, older adults, and people with disabilities may not have the inspiratory flows required to use a dry powder inhaler.[20] Pressurized metered-dose inhalers have unique clinical applications for specific patient groups.
In instances where pressurized metered-dose inhalers are deemed necessary, lower greenhouse gas emission per inhaler actuation could be used in preference to larger greenhouse gas emission per actuation. Based on our modeling analysis, conversion of all patients from high-volume to low-volume salbutamol pressurized metered-dose inhalers would theoretically reduce emissions by 3776 tCO2e (44%). A new propellant (HFA-152a) is currently in pharmaceutical development; it will reduce the carbon footprint of pressurized metered-dose inhalers by up to 90%, which will be equivalent to that of dry powder inhalers.[19] However, it is not yet known when pressurized metered-dose inhalers containing this propellant type will become clinically available.[19]
Cost must also be addressed when considering switching inhalers. Some switches from pressurized metered-dose inhalers to dry powder inhalers/soft mist inhalers are associated with a higher per-dose cost. Alternatives to pressurized metered-dose inhalers may not be readily available in BC because they may not be covered under the province’s PharmaCare program. However, the per-dose cost of pressurized metered-dose inhalers does not take into account the long-term cost of their climate impact and the associated health care costs due to poor respiratory control. Figure 3 shows the common pressurized metered-dose inhalers that are available in BC, along with their dry powder inhaler/soft mist inhaler counterpart, the PharmaCare coverage status, and the approximate cost of each inhaler.
Study limitations
Inhaler dispensing data may not reflect actual medication use. Patients may store inhalers for future use; thus, our calculation of overuse of short-acting ß2-agonists is likely an overestimate. However, our study does not account for in-hospital data; thus, the inhaler carbon footprint is underestimated. Additionally, patients older than 40 years of age who had asthma were excluded from our analysis of overuse of short-acting ß2-agonists. Finally, our scenarios for switching inhalers to lower-carbon alternatives are inexact. Our calculation of dose-to-dose conversion presumes equivalent efficacy across medications under the same class, which could introduce errors.
Conclusions
Climate change presents severe health consequences for all British Columbians. Therefore, there is an urgent need for all sectors, including health care, to decarbonize. The propellants used in pressurized metered-dose inhalers are potent greenhouse gases. With widely available alternatives for the management of asthma and chronic obstructive pulmonary disease, switching away from pressurized metered-dose inhalers with high carbon footprints, when appropriate, would be a positive step toward a meaningful reduction in greenhouse gas emissions by the health care sector.
Acknowledgments
This study makes use of data made accessible by the Health Data Platform BC. The authors would like to acknowledge all data providers who make data and information available for research. All inferences, opinions, and conclusions drawn in this article are solely those of the authors, not the Province of BC or data contributors. The authors would also like to thank Tate Goodman for his work in helping analyze the carbon footprint data.
Competing interests
None declared.
This article has been peer reviewed.
 |
| This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. |
References
1. Romanello M, McGushin A, Di Napoli C, et al. The 2021 report of the Lancet Countdown on health and climate change: Code red for a healthy future. Lancet 2021;398(10311):1619-1662.
2. Eckelman MJ, Sherman JD, MacNeill AJ. Life cycle environmental emissions and health damages from the Canadian healthcare system: An economic-environmental-epidemiological analysis. PLoS Med 2018;15:e1002623.
3. Watts N, Amann M, Arnell N, et al. The 2019 report of the Lancet Countdown on health and climate change: Ensuring that the health of a child born today is not defined by a changing climate. Lancet 2019;394(10211):1836-1878.
4. Fidler L, Green S, Wintemute K. Pressurized metered-dose inhalers and their impact on climate change. CMAJ 2022;194:e460.
5. Lavorini F, Corrigan CJ, Barnes PJ, et al. Retail sales of inhalation devices in European countries: So much for a global policy. Respir Med 2011;105:1099-1103.
6. Tennison I, Roschnik S, Ashby B, et al. Health care’s response to climate change: A carbon footprint assessment of the NHS in England. Lancet Planet Health 2021;5:e84-e92.
7. Janson C, Henderson R, Löfdahl M, et al. Carbon footprint impact of the choice of inhalers for asthma and COPD. Thorax 2020;75:82-84.
8. Fraser Health. About Fraser Health—Who we are and what we do. Accessed 15 July 2022. www.fraserhealth.ca/about-us/about-fraser-health.
9. Nwaru BI, Ekström M, Hasvold P, et al. Overuse of short-acting ß2-agonists in asthma is associated with increased risk of exacerbation and mortality: A nationwide cohort study of the global SABINA programme. Eur Respir J 2020;55:1901872.
10. Government of British Columbia. Health Data Platform BC. Accessed 2 January 2022. www2.gov.bc.ca/gov/content/health/conducting-health-research-evaluation/data-access-health-data-central/health-sector-partner-access-to-data/health-data-platform.
11. PrescQIPP Community Interest Company. Bulletin 295: Inhaler carbon footprint. Attachment 1. Accessed 1 January 2022. www.prescqipp.info/our-resources/bulletins/bulletin-295-inhaler-carbon-footprint.
12. Fraser Health Authority. 2021 public sector organization climate change accountability report—Fraser Health. Accessed 8 July 2022. www2.gov.bc.ca/assets/gov/environment/climate-change/cnar/2021/fraser_health_2021_ccar.pdf.
13. Kaplan A, van Boven JF, Ryan D, et al. GINA 2020: Potential impacts, opportunities, and challenges for primary care. J Allergy Clin Immunol Pract 2021;9:1516-1519.
14. Reddel HK, Bacharier LB, Bateman ED, et al. Global Initiative for Asthma strategy 2021: Executive summary and rationale for key changes. J Allergy Clin Immunol Pract 2022;10:S1-S18.
15. Bryant L, Bang C, Chew C, et al. Adequacy of inhaler technique used by people with asthma or chronic obstructive pulmonary disease. J Prim Health Care 2013;5:191-198.
16. Ramadan WH, Sarkis AT. Patterns of use of dry powder inhalers versus pressurized metered-dose inhalers devices in adult patients with chronic obstructive pulmonary disease or asthma: An observational comparative study. Chron Respir Dis 2017;14:309-320.
17. Conner JB, Buck PO. Improving asthma management: The case for mandatory inclusion of dose counters on all rescue bronchodilators. J Asthma 2013;50:658-663.
18. Barbara S, Kritikos V, Bosnic-Anticevich S. Inhaler technique: Does age matter? A systematic review. Eur Respir Rev 2017;26:170055.
19. Corr S. HFA-152a as a sustainable pMDI propellant. Resp Drug Delivery 2020;2:361-364.
Dr Liang is a family physician and clinical instructor in the Department of Family Practice at the University of British Columbia. Dr Yao is a regional epidemiologist for the British Columbia Centre for Disease Control. Dr Hui is a respirologist and clinical assistant professor in the Division of Respiratory Medicine, Department of Medicine, UBC. Mr Quantz is a public health consultant for the Fraser Health Authority.

Pharmacists in BC are very aware of this issue. However current regulations do not allow them to autosubstitute a dry powder inhaler for an MDI. Resolving this administrative logjam would go a long way to enabling these recommendations to be put into practice.