Workplace concussion recovery is everyone’s responsibility
Primary care providers have an important role in supporting patients in the early diagnosis and management of concussion-related symptoms, as well as their return to activity and function. According to WorkSafeBC data, there were 2754 work-related concussion claims that required ongoing benefits in 2023.[1]
An early and evidence-based approach by primary care to concussion, or mild traumatic brain injury (mTBI), can go a long way toward supporting injured workers in their return to function and work. One study found that up to 20% of those diagnosed with concussion experience persisting symptoms and related disability, impacting their quality of life and potentially delaying their return to work.[2] And it is estimated that one in six adults with concussion have symptoms that persist beyond 4 weeks.[3]
The importance of early intervention was highlighted in a recent pilot by WorkSafeBC. In 2021–2022, WorkSafeBC began an early referral pilot, in which injured workers with concussion were referred to the Early Concussion Assessment and Treatment program approximately 10 days earlier than when the program first began in 2020. Findings indicated that when workers received this early intervention even earlier, they were 3.1 times more likely to return to work within 12 weeks and 1.4 times more likely to return to work within 26 weeks. The data showed that this earlier intervention also decreased long-term sequalae, with 13% fewer referrals to long-term disability.
New clinical practice guideline for concussion
A new British Columbia clinical practice guideline, published in 2024, provides recommendations for the assessment, diagnosis, and management of concussion/mTBI that can be applied to all patients with concussion, including those with work-related concussion.[4]
The guideline provides resources on the diagnostic approach to concussion, the role of and approach to investigations, things to look for during follow-up screening and assessment, indications for referral, resources for symptom management and a gradual return to activity, and special considerations. Some key recommendations from the guideline are:
- Assess anyone with a suspected concussion as soon as possible, ideally within 72 hours, and before potential re-exposure to head trauma.
- Rule out serious injury (see Table 1, “Head injury red flags,” in the guideline).
- Confirm a diagnosis.
- Provide patient education and direct early management.
- Screen patients to identify those at risk of persisting symptoms.
- Evaluate patients for other conditions and manage these while also treating/managing concussion.
The guideline also recommends counseling patients about relative rest for the first 24 to 48 hours. It highlights the benefit of early activation and advising patients they can gradually return to activities even in the presence of mild symptoms, while avoiding activities that risk reoccurrence of head trauma. Providing written and verbal recommendations is also suggested. The Concussion Awareness Training Tool (CATT) has handouts for physicians that can help support your communication with patients. These and other resources are available at https://cattonline.com.
New legislation for BC employers and workers
Recent amendments to the Workers Compensation Act in BC include the legal duty that employers and workers have in working together to ensure a worker’s safe and timely return to work after any workplace injury, including concussion or mTBI. Employers with 20 or more workers also have a legal obligation to maintain employment of injured workers who have been employed for at least 12 months.[5] This means that employers must provide alternate or modified duties that allow injured workers to use current levels of functional abilities in the workplace.
Employers and workers are encouraged to collaborate in creating a safe and suitable return-to-work plan that includes a gradual, step-by-step process to return to pre-injury activity levels. This plan would begin based on the worker’s current abilities and include a modified schedule to allow for gradual reintegration and adaptation of more challenging tasks, as well as time to engage in symptom-management activities.
 Supporting your patient’s return to work
Supporting your patient’s return to work
In the clinic, supporting your patient’s return to work includes making an accurate assessment and diagnosis at the initial visit, regularly evaluating recovery progress and the patient’s tolerance of activities, encouraging them to follow safe increases in activity levels, and providing educational resources. As detailed in the BC Guideline on concussion/mTBI, a patient’s sleep and mood should also be considered and addressed. The guideline also refers to the association between high initial symptom severity and persisting symptoms. In addition, it is recommended that all patients have a primary care follow-up within 2 weeks of their diagnosis to screen for persisting symptoms and determine whether referrals to secondary care providers are needed.
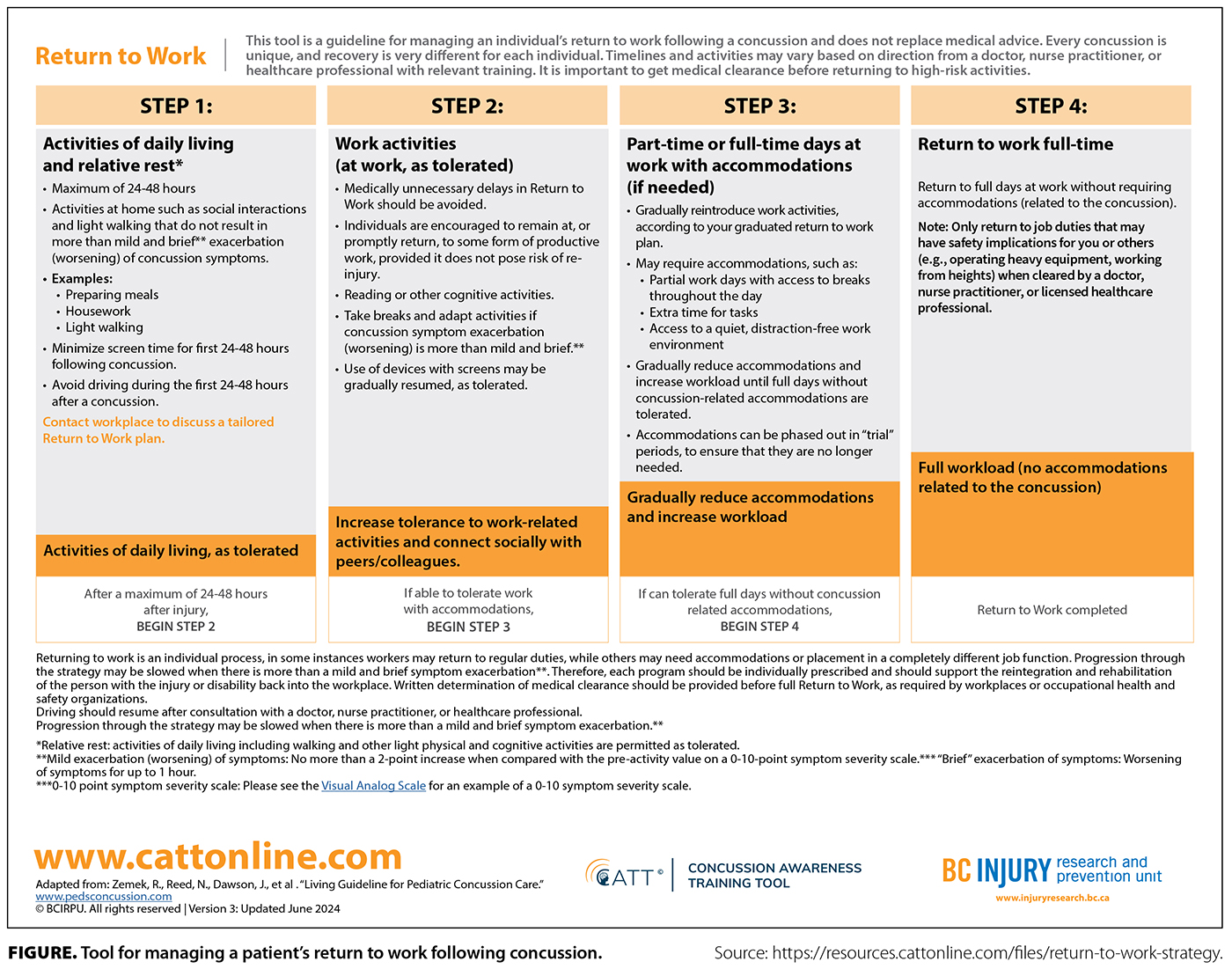
CATT and the BC Injury Research and Prevention Unit have developed a helpful resource that offers guidance for managing an individual’s return to work following concussion.[6] The four steps of the process help support a worker’s progress through a graduated return-to-work strategy [Figure].
More resources to help you support patients with work-related concussion
WorkSafeBC has two programs for workers who have accepted claims for work-related concussion.
The Early Concussion Assessment and Treatment program is delivered by a core team of a physical therapist and an occupational therapist, with additional support from a kinesiologist and a clinical counselor, as indicated. The primary focus of the program is early assessment, education, and focused intervention to facilitate an early and safe return to work and pre-injury function (www.worksafebc.com/en/health-care-providers/rehabilitation/early-concussion-assessment-treatment).
The Post-Concussion Management Program is an interdisciplinary outpatient program where workers receive individualized treatment plans that are implemented in a group environment. The plans are developed by a clinical team including a physician, a psychologist, a clinical counselor, a physical therapist, an occupational therapist, and a kinesiologist (www.worksafebc.com/en/health-care-providers/rehabilitation/post-concussion-management-program).
CATT also has additional resources for you and your patients, including the following e-learning courses:
- Concussion Awareness Training Tool for Medical Professionals (free and eligible for Mainpro+ and Maintenance of Certification credits): https://cattonline.com/course/concussion-awareness-training-tool-for-medical-professionals
- Concussion Awareness Training Tool for Workers and Workplaces: https://cattonline.com/course/concussion-awareness-training-tool-for-workers-and-workplaces
WorkSafeBC is here to support you. If you have questions or concerns about a patient with work-related concussion, speak with a WorkSafeBC medical advisor via the RACE app: www.raceconnect.ca/get-raceapp.
—Shelina Babul, PhD
Clinical Professor, Department of Pediatrics, University of British Columbia
Director, BC Injury Research and Prevention Unit
—Karen Takai
Program Manager, Health Care Programs, WorkSafeBC
—Olivia Sampson, MD
Manager, Medical Services, WorkSafeBC
hidden
This article is the opinion of WorkSafeBC and has not been peer reviewed by the BCMJ Editorial Board.
 |
| This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. |
References
1. WorkSafeBC. Statistics 2023. 9 December 2024. Accessed 16 May 2025. www.worksafebc.com/en/resources/about-us/annual-report-statistics/2023-statistics.
2. Committee on Sports-Related Concussions in Youth; Board on Children, Youth, and Families; Institute of Medicine; et al., editors. Treatment and management of prolonged symptoms and post-concussion syndrome. In: Sports-related concussions in youth: Improving the science, changing the culture. Washington, DC: National Academies Press (US), 2014. Accessed 8 May 2025. www.ncbi.nlm.nih.gov/books/NBK185342/.
3. Cancelliere C, Verville L, Stubbs JL, et al. Post-concussion symptoms and disability in adults with mild traumatic brain injury: A systematic review and meta-analysis. J Neurotrauma 2023;40:1045-1059. https://doi.org/10.1089/neu.2022.0185.
4. Government of British Columbia. Concussion/mild traumatic brain injury (mTBI). BC Guidelines. Revised 21 May 2025. Accessed 8 May 2025. www2.gov.bc.ca/gov/content/health/practitioner-professional-resources/bc-guidelines/concussion-mild-traumatic-brain-injury-mtbi.
5. WorkSafeBC. Bill 41: Amendments to the Workers Compensation Act. Accessed 16 May 2025. www.worksafebc.com/en/law-policy/workers-compensation-law/amendments/bill-41-amendments-to-the-workers-compensation-act.
6. Concussion Awareness Training Tool, BC Injury Research and Prevention Unit. Return to work. Updated June 2024. Accessed 8 May 2025. https://resources.cattonline.com/files/return-to-work-strategy.

