Road to recovery: A strategy to meaningfully address British Columbia’s substance use system of care
A call on communities to support this coordinated, accessible, and evidence-based approach for the first step toward recovery.
The need for a coordinated substance use system of care in British Columbia and beyond has never been more urgent. Since 2016, almost 50 000 Canadians have died from an opioid-related poisoning.[1] BC has been particularly affected, having the highest rates of opioid-poisoning deaths and hospitalizations for opioid and stimulant poisonings compared with the rest of Canada [Table].[1] 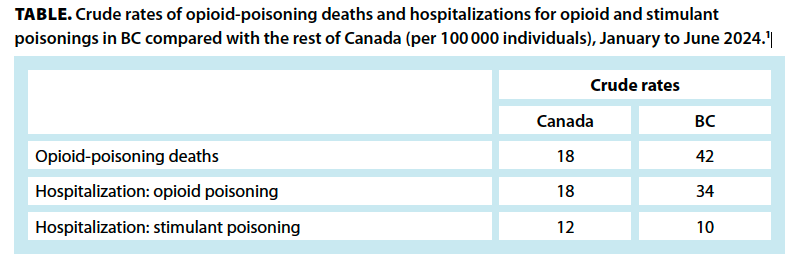
This burden of disease is not restricted to criminalized substances; alcohol misuse is also becoming a growing concern. Between 2015 and 2016, approximately 77 000 hospitalizations were attributable to alcohol-related harms (compared with 75 000 for heart attack).[2] While there have been initiatives to address the devastating consequences of substance use across the country, hospitalization and death rates continue to rise unabated.[1,2]
While reasons for the rise of substance-related hospitalization and death rates are multifactorial, in BC, the key contributors are the toxic nature of the drug supply combined with the siloed and fragmented addiction treatment system.[3] In 2022, the BC Coroners Service Death Review Panel and BC’s Select Standing Committee on Health urgently called for the creation of a coordinated substance use system of care.[4,5] Frontline health care providers agreed and highlighted two critical aspects of BC’s addiction treatment system that required urgent attention:
- An increase in the capacity to provide on-demand addiction care by trained health professionals.
- A reorganization and coordination of existing clinical services to ensure individuals with a substance use disorder could be seamlessly supported throughout their recovery.
To accomplish this, in a collaborative approach, the provincial government (specifically, the Ministries of Health and Mental Health and Addictions) and frontline health care providers in one health authority (a partnership between Providence Health Care and Vancouver Coastal Health [VCH]) began implementing a novel model of substance use care in September 2023. The Road to Recovery (R2R) initiative[6] addresses key aspects of BC’s recovery-oriented system of care to ensure that individuals can access on-demand and evidence-informed substance use services [Figure]. 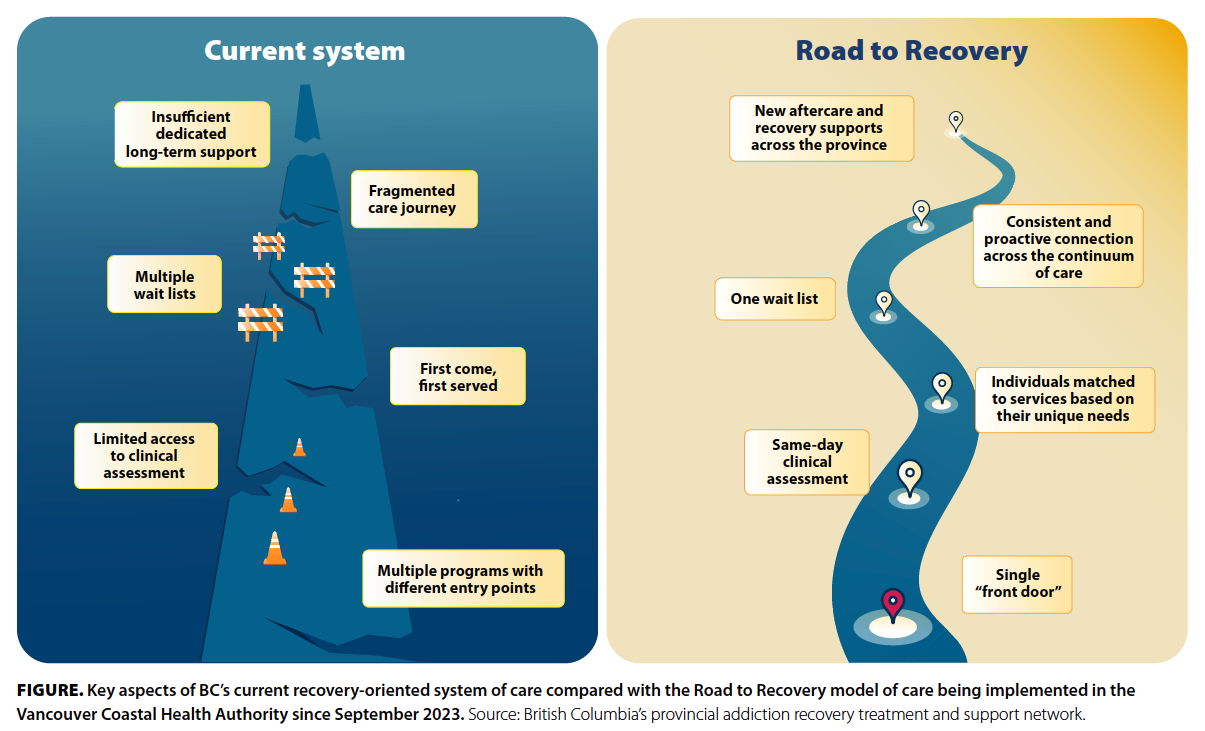
To increase capacity, almost 100 new addiction treatment beds will be added from 2023 to 2027, with 25 beds allocated to withdrawal management (i.e., detox) at or surrounding St. Paul’s Hospital (an acute care hospital near Vancouver’s Downtown Eastside, an area that experiences high rates of poverty, homelessness, mental illness, and substance use). The advantages of this approach include:
- Medically triaging individuals at highest risk for severe, complicated withdrawal (e.g., severe alcohol use disorder) to receive care in a higher-acuity medical facility (versus a community detox setting).
- Not occupying an acute care medical bed exclusively for withdrawal management.
- Admitting patients under the care of an interdisciplinary team with expertise in addiction medicine.
- Potentially linking individuals—many of whom may not otherwise engage with the health care system—to hospital-based general medical or surgical care (e.g., infectious disease or cardiac consultation for existing comorbidities).
- Offering primary prevention (i.e., screening) to a patient population that may be unattached to primary care services.
- Rapidly transferring individuals to a more medically supportive setting (i.e., intensive care) in a scenario of clinical decompensation.
An additional 20 net new transitional care (i.e., nonmedical) beds will also be created on the hospital’s campus. These beds will operate similarly to existing contracted beds in the region to facilitate easy transfers for individuals who may have stabilized from a withdrawal management perspective (either inpatient or outpatient) or who may not warrant a medical withdrawal management bed but require stabilization (e.g., stimulant use disorder, unstably housed, intensive outpatient treatment).
Finally, 50 additional recovery beds will be created near St. Paul’s Hospital, where individuals can focus on their recovery goals over a period of 3 to 6 months.
While increasing capacity is critical to meet the growing demand for substance use services in the VCH region, the more impactful work will result from optimizing efficiency in and between existing regional substance use services. Significant collaborative efforts are already underway to optimize access and coordinate existing VCH clinical services (e.g., medical withdrawal management, transitional care beds, bed-based recovery, aftercare supports) via the R2R initiative. R2R focuses on:
- Developing Access Central, the single point of access for all substance use services in the VCH region.
- Providing on-demand (i.e., same-day) addiction services virtually or in person.
- Ensuring an interdisciplinary team is available to support individuals when they access substance use care.
- Standardizing initial clinical assessment and individual care plans.
- Medically triaging individuals to ensure they receive the right level of care or acuity to manage their withdrawal syndrome (i.e., immediately transitioning those individuals at high risk for severe, complicated withdrawal to a medical withdrawal management bed and linking others to longitudinal, outpatient addiction services).
- Developing a single, centralized, regional wait list for access to bed-based substance use services (e.g., withdrawal management, transitional care beds, bed-based recovery services).
- Implementing proactive follow-up strategies to continuously engage and support individuals at transition points along their recovery.
The region’s commitment to truth and reconciliation with Indigenous Peoples is embedded in the R2R model of care. This commitment takes direction from the calls to action of the Truth and Reconciliation Commission of Canada, specifically to recognize the value of Indigenous healing practices and use them in the treatment of Indigenous patients; the calls for justice of the National Inquiry into Missing and Murdered Indigenous Women and Girls, a call for Indigenous-led health and wellness programs; and the In Plain Sight report, BC’s investigation into racism in the health care system, which speaks of hardwiring Indigenous cultural safety into health care and increasing access to culturally safe mental health and wellness and substance use services.
Indigenous patients make up approximately half of all admissions to the R2R unit at St. Paul’s Hospital. R2R has developed a collaborative, innovative, and multidimensional approach with the Indigenous Wellness and Reconciliation team. It includes Indigenous cultural safety education for providers, offers cultural services via Indigenous wellness liaisons, and shares data governance of Indigenous patient data generated within R2R.
In July 2024, the provincial government announced funding to implement and expand R2R to all regional health authorities.[7] This will advance progress toward creating a provincial model of substance use care, similar to what exists for the management of other chronic, relapsing diseases (e.g., renal care, cardiac care). Coordination of service delivery at the regional level will allow for common standards of care, access to high-quality evidence-based addiction care in any community, and, most importantly, the ability for care plans to follow a patient if they move within BC’s health authorities.
R2R offers a coordinated, accessible, and evidence-based approach for those looking to take their first step toward recovery, however that may be defined. While additional strategies to curb the ongoing toxic drug crisis, such as access to a safe drug supply, are still needed, we call on all communities across BC and beyond to support this innovative model of substance use care to ensure our loved ones can access the care they so deserve.
Competing interests
None declared.
Acknowledgments
Dr Dennis is supported by the Michael Smith Health Research BC–British Columbia Centre on Substance Use Partnered Scholar Award and the Providence Health Care Carraresi Foundation Early Career Clinician Investigator Award. Dr Nolan is funded by UBC’s Steven Diamond Professorship in Addiction Care Innovation.
The authors acknowledge the exceptional collaboration that has occurred to date to develop and implement R2R. Specifically, the provincial government has provided annual operating funding, and BC’s philanthropic community has helped fund capital refurbishments and start-up costs. Additionally, a huge team of operational and clinical leaders from Providence Health Care and its Indigenous Wellness and Reconciliation team, the Vancouver community, and the VCH Regional Addiction Program have worked tirelessly to implement R2R in the VCH region.
Last, the authors thank the individuals with lived and living experience of substance use and their loved ones for the abundance of inspiration and motivation they have provided to enact systemic change to improve substance use service delivery across the region.
hidden
This article has been peer reviewed.
 |
| This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. |
References
1. Public Health Agency of Canada. Opioid- and stimulant-related harms in Canada. Updated 23 December 2024. Accessed 4 January 2025. https://health-infobase.canada.ca/substance-related-harms/opioids-stimulants/.
2. Canadian Institute for Health Information (CIHI). Alcohol harm in Canada: Examining hospitalizations entirely caused by alcohol and strategies to reduce alcohol harm. Ottawa, ON: CIHI, 2017. Accessed 15 February 2024. www.cihi.ca/sites/default/files/document/report-alcohol-hospitalizations-en-web.pdf.
3. BC Ministry of Mental Health and Addictions. A pathway to hope: A roadmap for making mental health and addictions care better for people in British Columbia. 2021. Accessed 15 February 2024. www2.gov.bc.ca/assets/gov/british-columbians-our-governments/initiatives-plans-strategies/mental-health-and-addictions-strategy/bcmentalhealthroadmap_2019web-5.pdf.
4. BC Coroners Service. BC Coroners Service Death Review Panel: A review of illicit drug toxicity deaths. 2022. Accessed 15 February 2024. www2.gov.bc.ca/assets/gov/birth-adoption-death-marriage-and-divorce/deaths/coroners-service/death-review-panel/review_of_illicit_drug_toxicity_deaths_2022.pdf.
5. Legislative Assembly of British Columbia. Closing gaps, reducing barriers: Expanding the response to the toxic drug and overdose crisis. 2022. Accessed 14 February 2024. www.leg.bc.ca/committee-content/3316/SSC-Health-Report_42-3_2022-11-01_Final.pdf.
6. British Columbia Centre on Substance Use. The road to recovery. Accessed 14 February 2024. www.bccsu.ca/road-to-recovery.
7. BC Ministry of Mental Health and Addictions. Innovative model of addictions care expands throughout BC [news release]. 22 July 2024. Accessed 5 November 2024. https://news.gov.bc.ca/releases/2024MMHA0038-001175.
hidden
Ms Wellar is an undergraduate student in the School of Kinesiology at Western University. Dr Dennis is an assistant professor in the Department of Medicine in the University of British Columbia Faculty of Medicine and a clinician scientist at the British Columbia Centre on Substance Use (BCCSU). Mr Partridge is an operations director with Vancouver Coastal Health and program lead for specialized substance use services in Vancouver. Dr Brar is a clinical assistant professor in the Department of Family Practice at UBC. Ms H. Johnson is an adjunct professor in the UBC School of Population and Public Health and vice president of the Indigenous Wellness and Reconciliation team at Providence Health Care. Ms C. Johnson is an adjunct professor in the School of Nursing at UBC and executive director of the BCCSU. Dr Nolan is an associate professor in the Department of Medicine at UBC, a clinician scientist at the BCCSU, and head of the Interdepartmental Division of Addiction Medicine at Providence Health Care.

liked the article