Novel treatment of spasticity: International success through collaborative care
 |
| Team members received a Victoria Hospitals Foundation Caring Spirit award from a grateful patient’s family. From left to right: Dr Mahdis Hashemi, physical medicine and rehabilitation (PMR) head of research; Dr Daniel Vincent, anesthesiologist and inventor of cryoneurolysis for spasticity; Mr Danny Gatenby, University of Victoria co-op student; Dr Paul Winston, PMR; Ms Julie Connor, administrative lead; and Ms Laura Schatz, BSc, research kinesiologist. |
In 2018, our small Victoria clinic won a $10 000 South Island Facility Engagement Initiative Society grant, with the audacious title “Creating a world-leading centre in novel treatment of spasticity through collaborative care.”[1] So began our journey to launch what is now an internationally acclaimed innovation program for patients with spasticity. Fast-forward 6 years, and our cryoneurolysis for spasticity protocol has entered the international nomenclature.
Our goal of being a global centre of innovation was attained via many further engagement grants and the licensing of dozens of physicians from outside BC by the College of Physicians and Surgeons of BC (CPSBC). Our tiny clinic has raised close to $1 million from donors to the Victoria Hospitals Foundation, industry partners, Island Health Research grants, and other awards, including the 2024 Medical Post Innovative Practice Award and the Victoria Hospitals Foundation Caring Spirit award. We have published over 30 peer-reviewed publications. Our Atlas of Ultrasound-Guided Nerve-Targeted Procedures for Spasticity sold nearly 900 copies in 2 years before being translated into Mandarin and Japanese. Over 200 000 people have streamed our documentaries (here is one example: https://youtu.be/hpuD2cv85E4). Our clinic is full of University of Victoria and University of British Columbia co-op students, UBC Flexible and Enhanced Learning (FLEX) research students, and medical students and residents from across Canada.
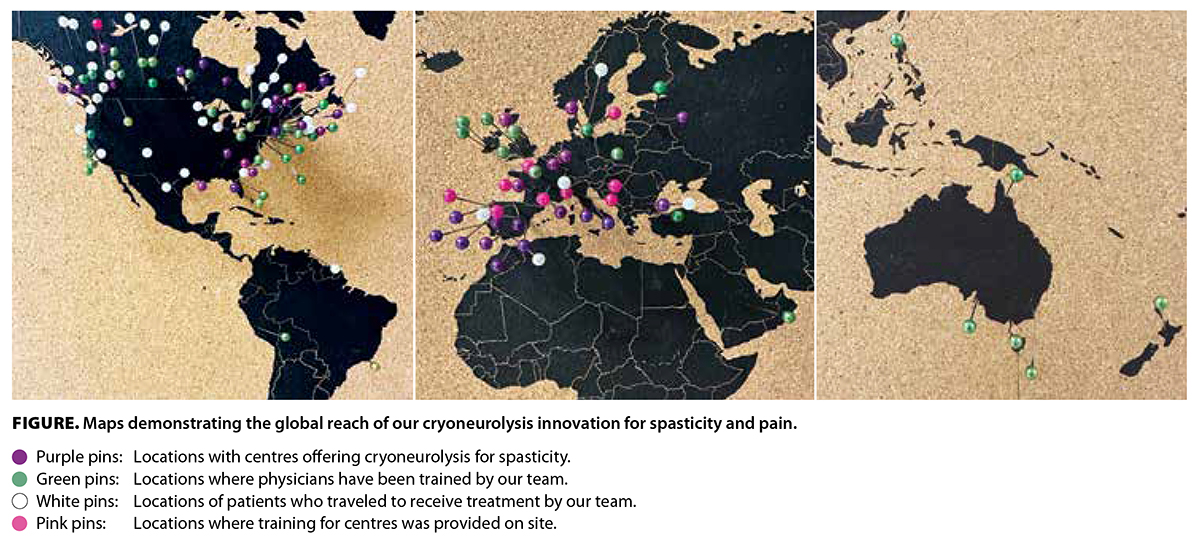 Each month, via our educational platform (https://arcryo.ca), up to five doctors from dozens of institutions around the world come to our patient treatment and training course, held in Victoria. Combined with the cities overseas where I have provided training, there are now centres worldwide [Figure] using our novel breakthrough treatment of freezing the nerves implicated in spasticity at temperatures as low as −88 °C. Clinics across North America and Europe, including at Harvard, Yale, and Oxford, and in Copenhagen and Luxembourg, offer the made-in-Victoria treatment. The CPSBC grants licences for patient care and works with physicians from all over the world. By allowing licensing for fellowships from 1 day to 6 months, access to educational opportunities around the world is streamlined.
Each month, via our educational platform (https://arcryo.ca), up to five doctors from dozens of institutions around the world come to our patient treatment and training course, held in Victoria. Combined with the cities overseas where I have provided training, there are now centres worldwide [Figure] using our novel breakthrough treatment of freezing the nerves implicated in spasticity at temperatures as low as −88 °C. Clinics across North America and Europe, including at Harvard, Yale, and Oxford, and in Copenhagen and Luxembourg, offer the made-in-Victoria treatment. The CPSBC grants licences for patient care and works with physicians from all over the world. By allowing licensing for fellowships from 1 day to 6 months, access to educational opportunities around the world is streamlined.
Through Doctors of BC and Island Health Research grants, we now treat children as young as 3 years old at Victoria General Hospital, with sedation support from the Division of Pediatrics; at Children’s Healthcare of Atlanta; and at the Hospital de Calahorra in La Rioja, Spain. Wascana Physiatry in Regina; Stanford Medicine Children’s Health Specialty Services in Sunnyvale, California; and Shriners Children’s Northern California will soon launch their own pediatric programs. A multicentre sham-controlled adult trial is also underway in the US. Our long-term care contracture study and nonoperative osteoarthritis initiatives and studies see patients well into their 90s.
The support from CPSBC and Doctors of BC is especially crucial. I am a UBC clinical faculty member, and most granting agencies do not favor applications from full-time clinicians. As we offer instantaneous changes to spastic muscle patterns, this ultrasound-guided procedure cannot be taught in a lab only. Our most recent facility engagement grants include virtual reality to reduce the pain of procedures and Indigenous visual storytelling to improve access to informed consent. With our anesthesia pain service grant, we created a mobile cryoneurolysis service for severe acute pain at two hospitals in Victoria, led by Dr Garrett Barry. One workshop attendee, Dr Michael Jew, launched a similar service at Providence Health Care in Vancouver. Dr Timothy Murray, an attendee from the Division of Radiology, is treating patients at St. Paul’s Hospital. We treat acute rib fractures and shoulder, hip, knee, and amputee pain, and we send patients home quickly.
In 2024, the Ministry of Health conducted an analysis of cost savings, led by Ms Barbara Tencer, prescription monitoring program manager, and found significant savings over an 18-month follow-up period for all patients evaluated. At the highest end, a spasticity patient can cost $9600 per year in medications, compared with $630 for the vast majority of patients treated with cryoneurolysis, who receive one treatment per year (double that amount if they have a second treatment). In addition, Providence Health Care has received funding from the Ministry of Health’s Innovation Pathway program (www.innovarium.org/en/putting-pain-ice-medical-innovation-changing-pain-management).
UBC clinical faculty on Vancouver Island face geographical disparity in access to research and educational support. UBC is not yet set up to offer distributed faculty the same access that is available to faculty in the Lower Mainland. Hence, funding from the Canadian Institutes of Health Research and similar agencies is currently geocentric to Vancouver. In contrast, funding from Doctors of BC is available equitably throughout the province.
Thanks to the support we’ve received from numerous dedicated organizations, we’ve treated over 1200 patients in Victoria. Every month, patients travel from across BC and the far reaches of North America to receive care. A commitment to innovation has changed lives around the world.
Our goals for the next several years are clear: no patient having to travel far to access this breakthrough drug-free therapy, an increase in opioid-free pain care, faster discharges, millions of dollars saved, and better patient outcomes. All backed by evidence and publications.
Acknowledgments
Dr Winston thanks the CPSBC and Doctors of BC for supporting knowledge translation and helping launch the clinic’s innovation program. He also gratefully acknowledges the support from Island Health and Island Health Research; the Victoria Hospitals Foundation; industry partners including Pacira BioSciences, AbbVie, and BioTalent Canada; the University of Victoria’s co-operative education program; UBC FLEX; the UBC Summer Student Research Program; and the Ministry of Health.
hidden
This article has been peer reviewed.
 |
| This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. |
References
1. BC Medical Journal. The Victoria Combined Peripheral Nerve and Spasticity Clinic. 2019;61:158,182.
hidden
Dr Winston is a clinical associate professor at the University of British Columbia and in the Island Medical Program.
Correction: This article has been revised. The author requested the following change postpublication: Dr Timothy Murray was incorrectly named as Dr Michael Murray.


Hey, I am doing a bit of research on cryoneurolysis and looking for anything you have on its impact on spasticity for children with CP. Has this or is this being studied?