Original Research
Surgical Patient Optimization Collaborative: A community hospital quality improvement perspective
Background: The surgical program at Peace Arch Hospital in White Rock, British Columbia, is committed to quality improvement and safety. To improve surgical outcomes, a multidisciplinary team enrolled in the Specialist Services Committee’s Surgical Patient Optimization Collaborative (SPOC) from January 2022 to July 2023. SPOC offers presurgical patient optimization processes to target comorbidities prior to surgery, which can lead to better patient outcomes.
Methods: We conducted a quality improvement project to provide optimization processes to 85% of presurgical patients who required them by focusing on smoking cessation, preoperative anemia investigation and treatment, social prescribing, and obstructive sleep apnea screening.
Results: SPOC optimization processes provided optimization to 90% of patients who required it and were associated with improved patient unplanned readmission rates, length of stay, and surgical site infection rates.
Conclusions: Overall, patients found the optimization processes improved their surgical experience.
Implementation of optimization processes in the surgical pre-admission process improved patient outcomes and surgical experiences.
Background
Patient comorbidities can contribute to surgical complications, but medical optimization can lead to better patient outcomes.[1] The terms preoperative optimization and prehabilitation describe optimization processes prior to surgery that are used to reduce the risk of complications such as myocardial events, pulmonary infection, wound infection, and impaired tissue healing.[2,3]
Peace Arch Hospital is a 201-bed community hospital in White Rock, British Columbia. Our surgical pre-admission process has been successful in identifying patient risks for poor surgical outcomes. However, prior to collaboration in the Specialist Services Committee’s Surgical Patient Optimization Collaborative (SPOC), we had limited formal standardized optimization processes to address these risk factors before surgery.
We conducted a quality improvement project with SPOC and our regional National Surgical Quality Improvement Program to test and implement standardized optimization processes in our surgical pre-admission process. Our aim was to successfully implement optimization processes to enable the optimization of 85% of presurgical patients who required it and to evaluate the effect on outcomes in patients who underwent elective arthroplasty procedures at our hospital from January 2022 to July 2023.
Methods
Setting
SPOC involves multiple hospital-based surgical programs within BC. It identifies several clinical areas for presurgical optimization and offers multiple ideas for screening and optimization for each area. Each hospital in the collaborative identified areas of optimization and customized its screening and optimization process accordingly. The provincial SPOC team designed 13 optimization processes to target drivers of perioperative complications and improve patient satisfaction: optimization of preoperative nutrition, social supports, anxiety, anemia, cardiac risk assessment, physical therapy, obesity, smoking cessation, substance abuse, frailty, pain management, obstructive sleep apnea, and glycemic control.
We conducted our project in the Surgery Pre-Admission Clinic at Peace Arch Hospital. We limited our project to elective arthroplasty patients. Peace Arch Hospital performs approximately 580 elective joint arthroplasties per year. Our project team included anesthesiologists, surgeons, Surgery Pre-Admission Clinic staff, hospital administrators, nurses, a patient partner, a sleep specialist, a project leader, and a family physician. Team meetings were held monthly to review testing of change ideas and implementation compliance and to plan adjustments to implementation strategies. Our team met with the provincial SPOC group every 3 months to receive instruction and reports from other hospitals in the collaborative.
 Design
Design
In keeping with the requirements of quality improvement, we used an analytic study because of the temporal nature of improvement. We relied on Shewhart charts and interpretation of common and special cause variation to assess our performance rather than statistical methods typically used with enumerative studies, such as hypothesis testing and confidence intervals.
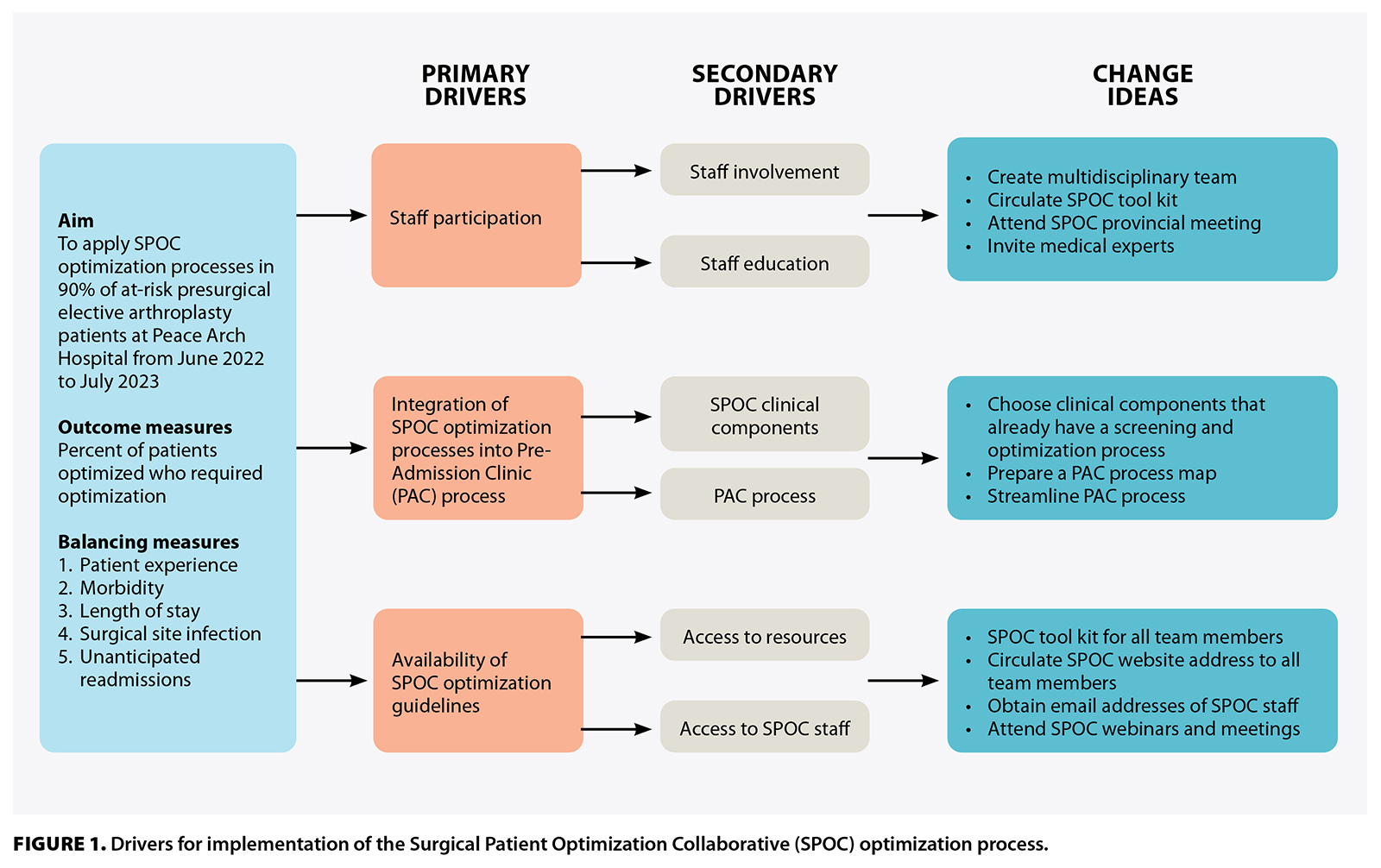
We used the Model for Improvement methodology to implement SPOC screening and optimization processes within the surgical pre-admission process. Our team developed a diagram to identify the primary drivers of implementing SPOC optimization processes and achieving successful optimization: staff participation, integration of SPOC processes into the Surgery Pre-Admission Clinic process, and availability of SPOC resources [Figure 1]. We used plan-do-study-act cycles to test change ideas that addressed the primary drivers of implementing optimization processes into our surgical pre-admission process.
Staff involvement
To promote staff engagement with the project, the SPOC optimization processes were presented in different ways to our staff. A SPOC tool kit was presented that outlined the guidelines of implementation and the rationale for the optimization processes. SPOC held several provincial meetings throughout the year to share different hospitals’ experiences in implementing the optimization processes. We invited several experts in the optimization processes to our monthly staff meetings to provide insight.
Integration of SPOC optimization processes into the clinic process
Our Surgery Pre-Admission Clinic staff were concerned about potential increased workloads with the integration of SPOC optimization processes into our clinical processes. To address this, we started by completing a process map for our surgical patient flow through our clinic. We eliminated redundant steps in this process to allow more time for screening and optimization. With key parties, we determined which optimization processes could be integrated without significant added workload and changes to the clinic process.
To increase compliance among clinic staff in delivering SPOC optimization processes, we implemented only four that had minimal impact on our pre-existing clinic process. Our pre-admission staff felt that these optimization processes were easy to accommodate into their workload and did not require significant additional time or staff. In addition, these optimization processes had clear endpoints for optimization, which allowed for easy follow-up by staff. The optimization processes were:
- Smoking cessation.
- Preoperative anemia investigation and treatment.
- Social prescription.
- Obstructive sleep apnea screening.
Smoking is associated with a significant increase in postoperative morbidity and mortality.[4] Many reviews and meta-analyses have demonstrated that preoperative smoking cessation improves outcomes.[5-7] Our intervention involved identifying smokers preoperatively using the preoperative patient questionnaire and our pre-existing preoperative baseline risk screen. Our clinic nurses informed these patients of the detrimental effects of continued smoking and the benefits of smoking cessation. The nurses also offered patients a referral to the QuitNow program if they wished to stop smoking preoperatively.
Preoperative anemia is an independent risk factor for worse outcomes in noncardiac surgery, including worse postoperative morbidity and infection rates and increased length of stay.[8] Anemic patients also have increased rates of perioperative acute kidney injury and transfusions. Evaluation and treatment of preoperative anemia are recommended to improve patient outcomes.[9] Our intervention involved defining preoperative anemia as hemoglobin less than 116 g/L. Our anesthesiologists collaborated with the patient’s family physician to evaluate and treat the anemia using recent national guidelines on the management of preoperative anemia.[9]
A patient’s social support is defined as those resources in a patient’s environment that enable the patient to cope with physical and psychological stresses.[10] Reliable patient social support networks at home are associated with improved recovery[11] and shorter length of stay in hospital.[12,13] The Fraser Health Authority Social Prescribing Program provides volunteers who help with transportation to medical appointments and with home errands. Our clinic nurses screened patients for lack of home support using discharge planning questions from the preoperative baseline screen. The nurses referred patients to the program if they concluded the patient would benefit from it.
Obstructive sleep apnea in surgical patients is associated with an increase in respiratory complications and length of stay in hospital.[14,15] It is also associated with other serious perioperative complications, including cardiac arrhythmia, myocardial injury, and sudden death.[16,17] To identify patients at high risk for obstructive sleep apnea prior to elective surgery, the STOP–Bang questionnaire is used as a validated screening tool.[18,19]
Screening for undiagnosed obstructive sleep apnea is recommended prior to surgery.[20] We used the STOP-Bang score within our preoperative patient questionnaire to screen for the risk of having severe obstructive sleep apnea. We used a STOP-Bang score of 3 or greater as an initial screen for obstructive sleep apnea. Our clinic nurse interviewed high-risk patients and gave them information about the effects of obstructive sleep apnea on surgical outcomes. Patients were referred to an anesthesiologist if they had symptoms of nighttime apnea, gasping, snoring, hypertension, or daytime somnolence. Subsequently, these patients were interviewed and sent for a home sleep apnea test or were referred to a sleep specialist using the BC Obstructive Sleep Apnea: Assessment and Management guidelines.[21] Continuous positive airway pressure (CPAP) was recommended if the patient was diagnosed with obstructive sleep apnea, because it has been shown to reduce complications in surgical patients with this condition.[15,22] Patient follow-up was coordinated with the patient’s family physician.
Availability of the optimization tool kit
Availability of the SPOC tool kit was essential to help staff in referencing optimization materials. We distributed booklets containing the SPOC optimization tool kit to all members of our team. The SPOC website, which contains the tool kit, was accessible online and through a QR code. Names of the care providers involved in creating the tool kit were made accessible to our staff.
Measures
Outcome measures
Our primary outcome measure was to determine the effectiveness of implementing the SPOC optimization process by measuring the percentage of patients who required optimization and received it. We defined a patient who required optimization as someone who had a history of one or more of the following: inadequate social support, preoperative anemia, current smoking, or high risk of obstructive sleep apnea. We defined optimized as any patient who received at least one optimization process. SPOC provided a pre-existing tool to measure this outcome in June 2022.
Balancing measures
Our balancing measures for patient outcomes included arthroplasty patients’ experience with the optimization process, morbidity rates, surgical site infection rates, unplanned readmission rates, and length of stay. We measured patients’ satisfaction by telephoning them 1 month after their surgical procedure and asking them two questions about their experience: (1) Was your surgical experience improved as a result of information/care pre-op? (2) Was your overall health improved as a result of the information/care pre-op? Baseline data for surgical site infection rates, morbidity rates, readmission rates, and length of stay were obtained from the National Surgical Quality Improvement Program. We continued using this program to collect data throughout the study period.
Process measures
We obtained process measures through chart reviews. They included the percentage of eligible patients who started on CPAP, the percentage of patients who quit smoking preoperatively, the percentage of anemic patients with improved hemoglobin levels, and the percentage of patients who accepted social supports.
Results
We screened 260 patients for prehabilitation; 137 needed one or more optimization processes offered through our Surgery Pre-Admission Clinic.
Outcome measures
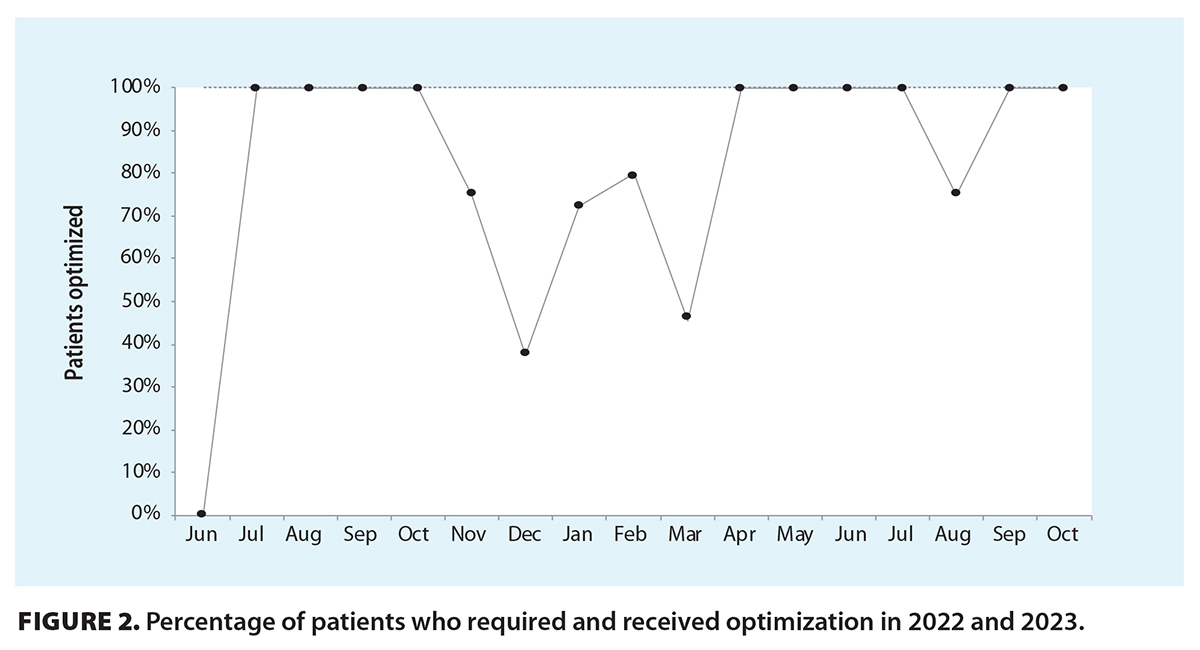 SPOC provided a process to collect data on the percentage of patients who required optimization and received it. We achieved 100% optimization from June to October [Figure 2]. However, these results were not sustainable, because our optimization processes resulted in a high nursing workload. The screening process for optimization contributed to the increase in workload. This resulted in a decline in optimization from October to December. From December to April, we conducted several plan-do-study-act cycles to streamline our optimization and screening process to reduce the impact on nursing. The largest improvement occurred in April, when we introduced a nurse navigator to screen patients and used email to disseminate educational information. As a result, our optimization rates improved from April to October. The percentage decline in August was due to common cause variation (i.e., normal variation in the process) since it was not sustained and did not show a trend.
SPOC provided a process to collect data on the percentage of patients who required optimization and received it. We achieved 100% optimization from June to October [Figure 2]. However, these results were not sustainable, because our optimization processes resulted in a high nursing workload. The screening process for optimization contributed to the increase in workload. This resulted in a decline in optimization from October to December. From December to April, we conducted several plan-do-study-act cycles to streamline our optimization and screening process to reduce the impact on nursing. The largest improvement occurred in April, when we introduced a nurse navigator to screen patients and used email to disseminate educational information. As a result, our optimization rates improved from April to October. The percentage decline in August was due to common cause variation (i.e., normal variation in the process) since it was not sustained and did not show a trend.
Balancing measures
We conducted 118 patient interviews to evaluate the patient experience with the optimization process; 70% of those patients felt their overall health had improved as a result of the information and care provided by the surgical preoperative team, and 93% reported that their surgical experience had improved.
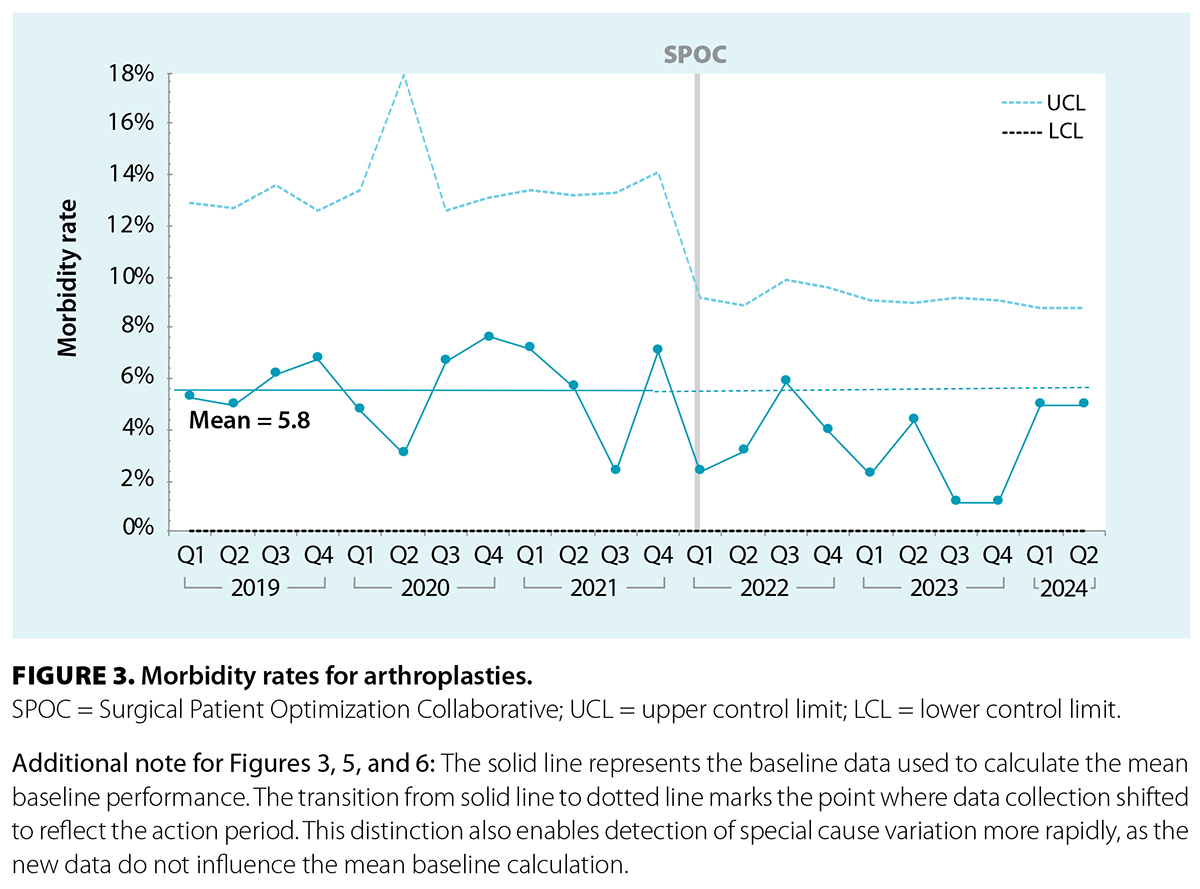
The baseline mean rate for morbidity was 5.8% [Figure 3]. Our rates did not reveal any special cause variation after starting SPOC processes; however, the upper control limits narrowed during the study.
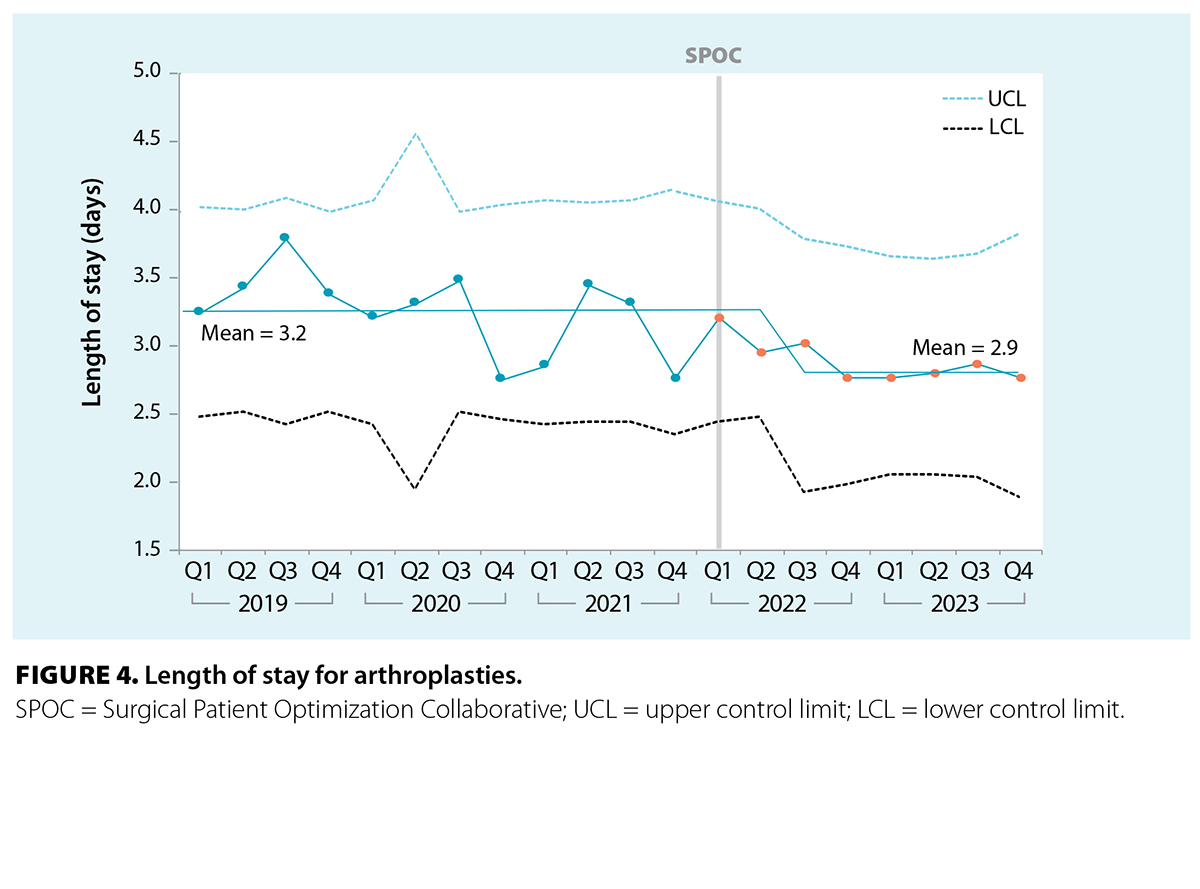
The baseline mean for arthroplasty length of stay was 3.2 days [Figure 4]. There was a special cause variation shift to below our baseline mean (to 2.9 days) after initiating SPOC processes, and the upper control limits narrowed.
 |
 |
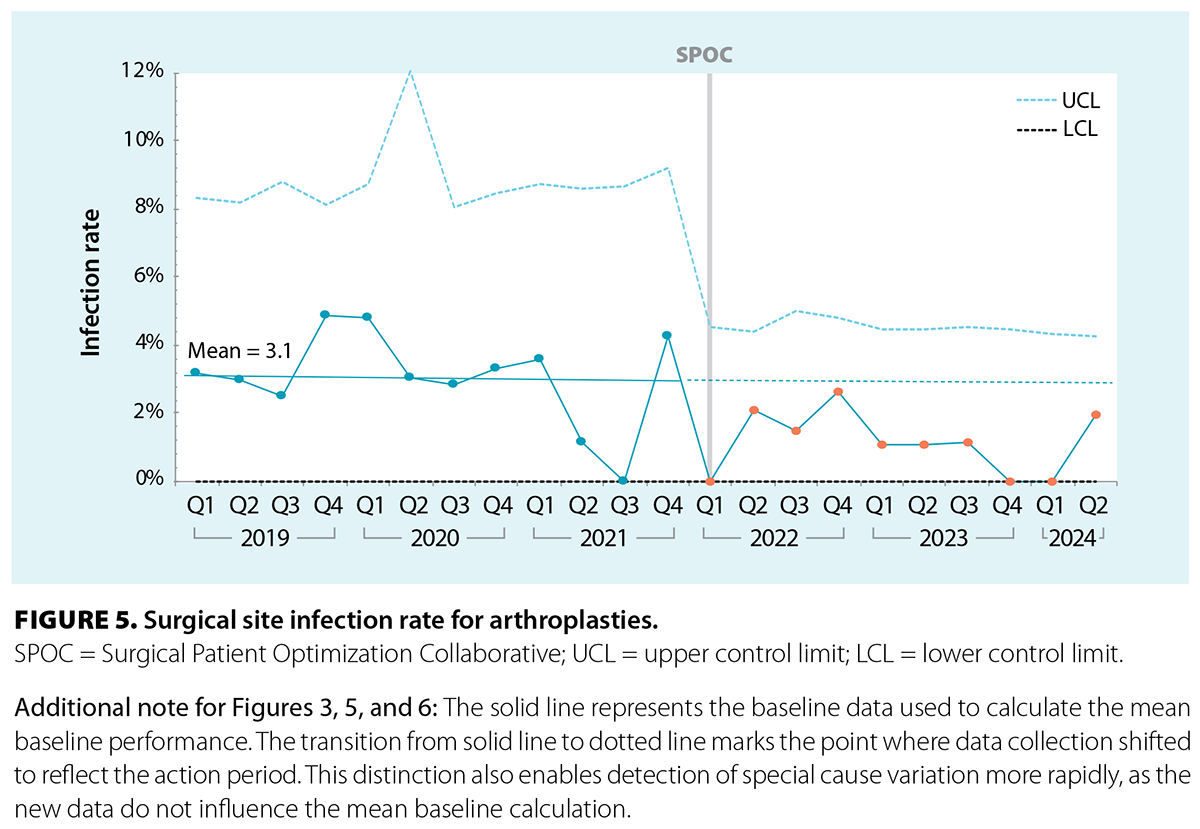
The baseline mean surgical site infection rate was 3.1% [Figure 5]. A special cause variation shift to improvement occurred after SPOC processes were initiated (the mean declined to 1.1%), and the upper control limits narrowed.
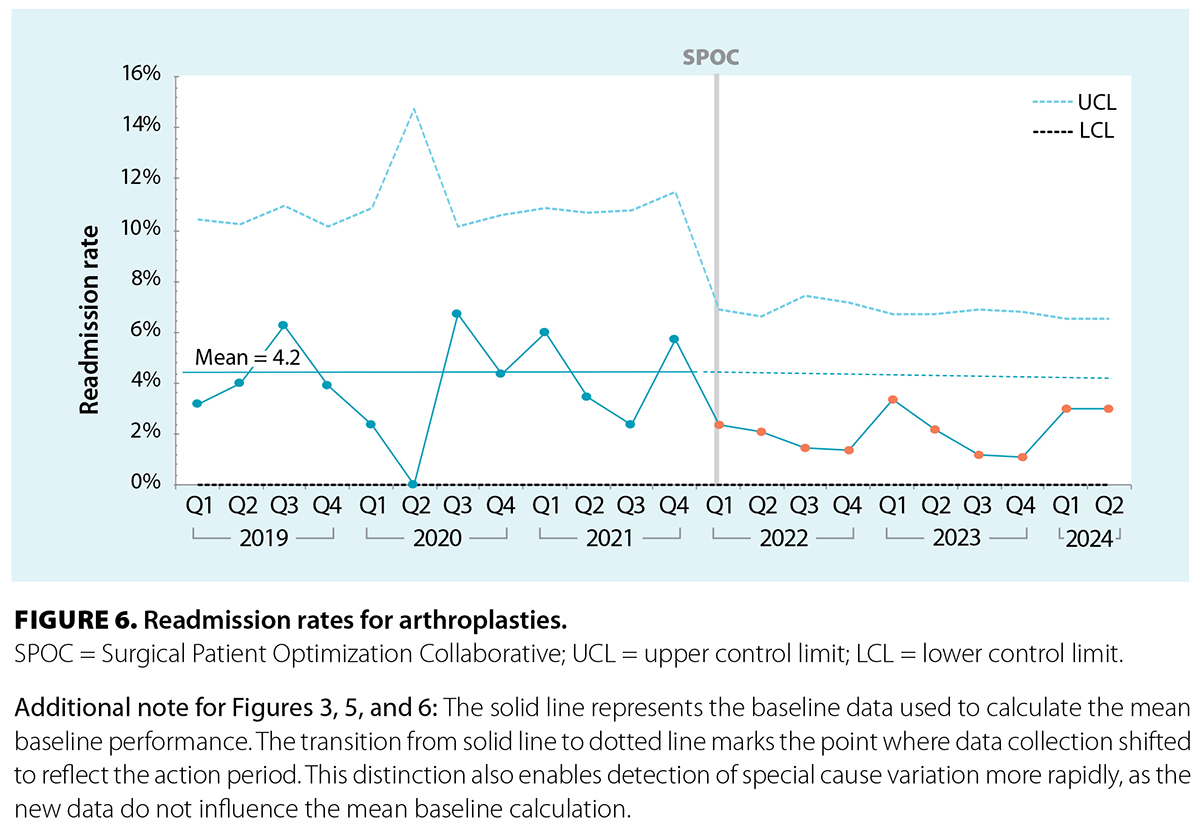
The baseline mean readmission rate for arthroplasties was 4.2% [Figure 6]. There was a special cause shift to below the baseline mean (to 2.2%) after SPOC processes were initiated, and the upper control limits narrowed.
 |
 |
Process measures
Thirty-two patients were at high risk for obstructive sleep apnea; 27 (84.4%) completed obstructive sleep apnea testing before surgery, and 17 (63.0%) tested patients started CPAP before surgery. Of 23 smokers, 19 (82.6%) who were offered prehabilitation quit or reduced their smoking before surgery. We did not follow their smoking history after surgery. Eleven patients were identified as anemic; eight (72.7%) who required optimization had improved hemoglobin preoperatively. Sixty patients were referred to the Social Prescribing Program; 19 (31.7%) did not require social supports postoperatively. Forty-eight of the referred patients answered our postoperative survey questions; 25 (52.1%) agreed that social support was helpful to their postoperative recovery.
Conclusions
Preoperative optimization of patients’ comorbidities is important. Before our involvement with SPOC, our optimization of medical risk factors in presurgical patients was inconsistent and nonstandardized. This presented an opportunity to use quality improvement methodology to implement standardized optimization processes and to assess effects on patient outcomes. We successfully implemented optimization processes in our surgical pre-admission process for providing social supports, preoperative management of anemia and obstructive sleep apnea risk, and smoking cessation. We were able to customize SPOC processes to allow them to be integrated into our existing workflow with minimal disruption. This led to a high compliance rate for optimization processes among Surgery Pre-Admission Clinic staff. A nurse navigator proved useful in screening patients for optimization.
Overall, patients found the optimization processes improved their surgical experience. Patients were motivated to pursue actions to improve their surgical outcomes. High-risk obstructive sleep apnea patients were willing to undergo testing to confirm their condition. Smokers were willing to stop or reduce smoking prior to surgery. Anemic patients were willing to undergo investigations and take supplemental iron if necessary. We felt that we were successful in providing social supports for patients with inadequate support at home. Our screening for the Social Prescribing Program did not have standardized criteria for referral. Referrals were made at the discretion of the screening nurse, but 31.7% of patients referred to the program did not require support at home. We believe this result can be improved by implementing formalized criteria for referrals.
After implementing standardized approaches to optimization in our clinic process, length of stay, unplanned readmissions, and surgical site infection rates improved. The initiation of SPOC processes was not associated with any special cause variation in morbidity rates; therefore, we plan to explore other approaches to reduce those rates. In all patient outcomes, upper control limits narrowed after initiating SPOC processes. We believe this represents a decrease in system variability, which is attributed to greater standardization of the optimization process. These results highlight the importance of having a structured, embedded optimization process within the surgical pre-admission process.
We believe the high workload on the nurse navigator for screening and optimization activities limited the ability to expand the program to other elective surgeries or other sites without large increases in human resources within our clinic.
It may be possible to improve capacity for optimization in the future without adding more human resources by increasing the use of digital tools for screening and identifying optimizable opportunities. Since a substantial amount of our clinic nursing resources are devoted to screening for medical history and making decisions about preoperative testing, leveraging a digital tool to algorithmically assist in those tasks may free capacity for clinic nurses to perform nurse navigator duties. In one study, switching to a digital questionnaire reduced nurse assessment times by more than 50%.[23] With more of our clinic nurses engaging with patients in optimization, there would be increased potential for widespread uptake of health improvements preoperatively. Several reports have described the potential for technology to enhance preoperative screening and medical optimization.[24-27] Self-administered detailed screening questionnaires have been found to be acceptable to patients and reliable in eliciting a medical history.[28] A review of digital technologies for promoting positive preoperative behavior changes found that technology should provide motivation and support, enable patient engagement, facilitate peer networking, and meet individualized patient needs.[29] The provincial Perioperative Care Alignment and Digital Screening committee, consisting of anesthesiologists, surgeons, internists, family doctors, Surgery Pre-Admission Clinic personnel, and patients, has been working on a digital tool that might assist with preoperative optimization in BC. The aim is to provide every presurgical patient with digitally supported, individually tailored, evidence-based advice, referrals, and recommendations before surgery. Until a digital solution is widely adopted, Peace Arch Hospital will maintain the optimization pathways that were successfully developed during the SPOC project period and will continue to find ways to expand using current resources.
Competing interests
None declared.
This article has been peer reviewed.
 |
| This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. |
References
1. Dlott CC, Moore A, Nelson C, et al. Preoperative risk factor optimization lowers hospital length of stay and postoperative emergency department visits in primary total hip and knee arthroplasty patients. J Arthroplasty 2020;35:1508-1515.e2. https://doi.org/10.1016/j.arth.2020.01.083.
2. Durrand J, Singh SJ, Danjoux G. Prehabilitation. Clin Med 2019;19:458-464. https://doi.org/10.7861/clinmed.2019-0257.
3. McIsaac DI, Gill M, Boland L, et al. Prehabilitation in adult patients undergoing surgery: An umbrella review of systematic reviews. Br J Anaesth 2022;128:244-257. https://doi.org/10.1016/j.bja.2021.11.014.
4. Møller AM, Villebro N, Pedersen T, Tønnesen H. Effect of preoperative smoking intervention on postoperative complications: A randomised clinical trial. Lancet 2002;359(9301):114-117. https://doi.org/10.1016/S0140-6736(02)07369-5.
5. Theadom A, Cropley M. Effects of preoperative smoking cessation on the incidence and risk of intraoperative and postoperative complications in adult smokers: A systematic review. Tob Control 2006;15:352-358. https://doi.org/10.1136/tc.2005.015263.
6. Mills E, Eyawo O, Lockhart I, et al. Smoking cessation reduces postoperative complications: A systematic review and meta-analysis. Am J Med 2011;124:144-154.e8. https://doi.org/10.1016/j.amjmed.2010.09.013.
7. An D, Wong J. Improving surgical outcomes and patient health: Perioperative smoking cessation interventions. Curr Anesthesiol Rep 2020;10:12-18. https://doi.org/10.1007/s40140-020-00370-0.
8. Viola J, Gomez MM, Restrepo C, et al. Preoperative anemia increases postoperative complications and mortality following total joint arthroplasty. J Arthroplasty 2015;30:846-848. https://doi.org/10.1016/j.arth.2014.12.026.
9. Greenberg JA, Zwiep TM, Sadek J, et al. Clinical practice guideline: Evidence, recommendations and algorithm for the preoperative optimization of anemia, hyperglycemia and smoking. Can J Surg 2021;64:E491-E509. https://doi.org/10.1503/cjs.011519.
10. Fitzgerald JD, Orav EJ, Lee TH, et al. Patient quality of life during the 12 months following joint replacement surgery. Arthritis Rheum 2004;51:100-109. https://doi.org/10.1002/art.20090.
11. Brembo EA, Kapstad H, Van Dulmen S, Eide H. Role of self-efficacy and social support in short-term recovery after total hip replacement: A prospective cohort study. Health Qual Life Outcomes 2017;15:68. https://doi.org/10.1186/s12955-017-0649-1.
12. Mitchinson AR, Kim HM, Geisser M, et al. Social connectedness and patient recovery after major operations. J Am Coll Surg 2008;206:292-300. https://doi.org/10.1016/j.jamcollsurg.2007.08.017.
13. Wylde V, Kunutsor SK, Lenguerrand E, et al. Is social support associated with patient-reported outcomes after joint replacement? A systematic review and meta-analysis. Lancet Rheumatol 2019;1:e174-e186. https://doi.org/10.1016/s2665-9913(19)30050-5.
14. Memtsoudis S, Liu SS, Ma Y, et al. Perioperative pulmonary outcomes in patients with sleep apnea after noncardiac surgery. Anesth Analg 2011;112:113-121. https://doi.org/10.1213/ANE.0b013e3182009abf.
15. Gupta RM, Parvizi J, Hanssen AD, Gay PC. Postoperative complications in patients with obstructive sleep apnea syndrome undergoing hip or knee replacement: A case-control study. Mayo Clin Proc 2001;76:897-905. https://doi.org/10.4065/76.9.897.
16. Porhomayon J, Nader ND, Leissner KB, El-Solh AA. Respiratory perioperative management of patients with obstructive sleep apnea. J Intensive Care Med 2014;29:145-153. https://doi.org/10.1177/0885066612446411.
17. Adesanya AO, Lee W, Greilich NB, Joshi GP. Perioperative management of obstructive sleep apnea. Chest 2010;138:1489-1498. https://doi.org/10.1378/chest.10-1108.
18. Chudeau N, Raveau T, Carlier L, et al. The STOP-BANG questionnaire and the risk of perioperative respiratory complications in urgent surgery patients: A prospective, observational study. Anaesth Crit Care Pain Med 2016;35:347-353. https://doi.org/10.1016/j.accpm.2016.01.006.
19. Hwang M, Nagappa M, Guluzade N, et al. Validation of the STOP-Bang questionnaire as a preoperative screening tool for obstructive sleep apnea: A systematic review and meta-analysis. BMC Anesthesiol 2022;22:366. https://doi.org/10.1186/s12871-022-01912-1.
20. American Society of Anesthesiologists Task Force on Perioperative Management of Patients with Obstructive Sleep Apnea. Practice guidelines for the perioperative management of patients with obstructive sleep apnea: An updated report by the American Society of Anesthesiologists Task Force on Perioperative Management of Patients with Obstructive Sleep Apnea. Anesthesiolology 2014;120:268-286. https://doi.org/10.1097/ALN.0000000000000053.
21. Government of British Columbia. Obstructive sleep apnea: Assessment and management in adults. Updated 19 September 2023. www2.gov.bc.ca/gov/content/health/practitioner-professional-resources/bc-guidelines/sleep-apnea.
22. Liao P, Yegneswaran B, Vairavanathan S, et al. Postoperative complications in patients with obstructive sleep apnea: A retrospective matched cohort study. Can J Anaesth 2009;56:819-828. https://doi.org/10.1007/s12630-009-9190-y.
23. Taylor SK, Andrzejowski JC, Wiles MD, et al. A prospective observational study of the impact of an electronic questionnaire (ePAQ-PO) on the duration of nurse-led pre-operative assessment and patient satisfaction. PLoS One 2018;13:e0205439. https://doi.org/10.1371/journal.pone.0205439.
24. Durrand JW, Moore J, Danjoux G. Prehabilitation and preparation for surgery: Has the digital revolution arrived? Anaesthesia 2022;77:635-639. https://doi.org/10.1111/anae.15622.
25. Durrand J, Livingston R, Tew G, et al. Systematic development and feasibility testing of a multibehavioural digital prehabilitation intervention for patients approaching major surgery (iPREPWELL): A study protocol. PLoS One 2022;17:e0277143. https://doi.org/10.1371/journal.pone.0277143.
26. Blumenau Pedersen M, Saxton J, Birch S, et al. The use of digital technologies to support home-based prehabilitation prior to major surgery: A systematic review. Surgeon 2023;21:e305-e315. https://doi.org/10.1016/j.surge.2023.05.006.
27. Powley N, Tew GA, Durrand J, et al. Digital health coaching to improve patient preparedness for elective lower limb arthroplasty: A quality improvement project. BMJ Open Qual 2023;12:e002244. https://doi.org/10.1136/bmjoq-2022-002244.
28. Osman T, Lew E, Lum EP-M, et al. PreAnaesThesia computerized health (PATCH) assessment: Development and validation. BMC Anesthesiol 2020;20:286. https://doi.org/10.1186/s12871-020-01202-8.
29. Robinson A, Oksuz U, Slight R, et al. Digital and mobile technologies to promote physical health behavior change and provide psychological support for patients undergoing elective surgery: Meta-ethnography and systematic review. JMIR Mhealth Uhealth 2020;8:e19237. https://doi.org/10.2196/19237.
Dr Cheng is an assistant professor of anesthesiology at the University of British Columbia and a staff anesthesiologist and physician quality lead at Peace Arch Hospital. Dr Lee is an assistant professor of anesthesiology at UBC and teaching faculty with the Fraser Health Authority Physician Quality Improvement training program. Ms Tecson is a director for the Fraser Health Authority Surgical Safety Program and Physician Partnerships. Ms Panesar is a leader for the Fraser Health Authority National Surgical Quality Improvement Program.
