Review Articles
In-office management of knee osteoarthritis
ABSTRACT: Nonsurgical management of knee osteoarthritis should be used in less severe disease cases or while patients await total knee arthroplasty. Bracing appears to improve function, pain management, and quality of life, but further high-quality research is needed. We recommend using unloader braces specifically in unicompartmental osteoarthritis; however, patient compliance is imperative to achieve the benefits. The safety, efficacy, and benefits of topical applications of NSAIDs are well outlined in the literature, and their use should be considered in knee osteoarthritis. Further study is needed to assess the efficacy of topical applications of capsaicin and herbal remedies, such as Hedera helix, and clinical trials on the use of cannabis to manage osteoarthritis pain have yet to be reported in the literature. There is substantial evidence that corticosteroid injections are beneficial for short-term pain relief in knee osteoarthritis. Viscosupplementation may have a role in the office setting, but it is not currently recommended for routine usage due to a lack of data showing clinically relevant differences associated with its use. Currently, there is not enough evidence to support the routine use of mesenchymal stem cell injections for osteoarthritis management, and the cost is significantly higher than that of alternative therapies.
Treating knee osteoarthritis in the clinic using unloader braces, topical applications of NSAIDs, and intra-articular corticosteroid injections can help improve function and pain management.
Knee osteoarthritis is a degenerative condition that results from progressive loss of articular cartilage, usually in the setting of chronic wear and tear or many years after trauma that has caused articular irregularity. Currently, 3.9 million Canadians over the age of 20 years have been diagnosed with osteoarthritis.[1] The economic burden of arthritis in Canada has been estimated to be more than $6.4 billion.[2] Patients typically experience knee pain that is often gradual, increases with activity, and leads to swelling and pain that gets worse over time.[3] The definitive surgical management for this condition when pain and disability are recalcitrant to other forms of treatment is a total knee replacement. However, before surgery is considered, many different treatment modalities, ranging in invasiveness from knee braces and topical treatments to intra-articular injections, can be used in the office setting to treat knee osteoarthritis.
Unloader braces
In the setting of unicompartmental knee osteoarthritis, there is often a coronal malalignment that leads to an increased mechanical load on the medial or lateral compartments. Knee bracing via unloader braces is a conservative option that offers mechanical unloading in the coronal plane to counteract the plane of the deformity driving the pathology.[4] For example, symptoms due to isolated medial compartment osteoarthritis in the setting of a varus lower limb malalignment will often be improved with a valgus-producing force that can be applied using an unloader brace. Bracing is a safe and noninvasive option, but it requires patient adherence over a long period to be efficacious. The literature indicates that brace treatment can be used to improve function, quality of life, and pain; however, there is heterogeneity in studies and a lack of high-quality studies.
In a multicentre RCT that involved 117 patients, the effects of unloader braces in unicompartmental osteoarthritis were analyzed; pain severity and knee function scores were improved with bracing.[5] Additionally, the bracing group had an increased walking distance at 3 and 12 months (P = .03 and P = .04, respectively).[5] It was concluded that bracing was effective.
The effects of unloading braces were also examined in an RCT conducted with 67 patients who presented with medial knee osteoarthritis.[6] The offloading brace was worn for 6 weeks; the brace group had a statistically significant reduction in 24-hour pain (P < .0001) and better functional outcomes based on the Lequesne index score (P < .0001).[6] It was concluded that unloading knee braces were effective in improving motion and global pain in the setting of medial knee osteoarthritis.[6] The benefits of unloader braces were also confirmed by an RCT that involved 119 patients. It showed that unloader bracing led to improvements in quality of life (P = .001) and function (P < .001) for patients with varus gonarthrosis.[7] Another study examined whether unloading braces were a cost-effective method for bridging and postponing surgery in unicompartmental knee osteoarthritis.[8] It indicated that unloading braces were cost-effective for the management of unicompartmental osteoarthritis and were beneficial for the capacity, budget, wait-list length, frequency, and required severity of surgical intervention.[8] In contrast, a meta-analysis of 14 systematic reviews and 9 RCTs brought into question the efficacy of unloader braces.[9] It suggested that the use of unloader knee braces likely increases physical function through walking distance, but its efficacy for quality of life and pain was questioned.[9] The study acknowledged the lack of homogeneity in the studies reviewed in regard to the type of brace, protocol, and outcome measures.[9] Bracing appears to improve function, pain, and quality of life; however, further high-quality research is needed. We recommend the use of unloader braces specifically in the setting of unicompartmental osteoarthritis, but patient compliance is imperative to achieve the mentioned benefits.
Topical treatments
Topical applications of NSAIDs have been a mainstay in the treatment of osteoarthritis.[10] They function by inhibiting the production of prostaglandins, which leads to anti-inflammatory and analgesic effects.[10] A number of high-quality studies have indicated that NSAIDs are effective in improving function and quality of life and have few or no adverse events in patients with knee osteoarthritis.[11-14] In an RCT that compared diclofenac with controls in 216 patients with knee osteoarthritis, diclofenac usage resulted in improvements in pain, physical function, and stiffness (P = .003, P = .0001, and P = .002, respectively).[11] Despite finding that 39% of the topical diclofenac group (consisting of 1.5% w/w diclofenac sodium) suffered from local skin dryness and skin irritation, it was concluded that topical NSAIDs were safe and efficacious for knee osteoarthritis.[11] A large multicentre RCT with 1395 patients assessed the efficacy and safety of topical ketoprofen and oral celecoxib.[12] Topical ketoprofen was superior to oral placebo and was considered to be noninferior to celecoxib with regard to pain based on the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC).[11] Similar results were found in an RCT with 248 patients in which topical diclofenac was compared with a placebo solution.[13] The study’s primary endpoint was pain relief, measured by the WOMAC, and it indicated that diclofenac was superior in reducing pain and stiffness and increasing physical function.[13] Although 36% of the diclofenac patients had minor local skin irritation, it was concluded that topical diclofenac provided safe treatment with minimal systemic side effects.[13] The efficacy of topical NSAIDs was further confirmed in an RCT with 260 patients; the topical NSAIDs group had a greater reduction in WOMAC pain scores (P = .04) and a minimal increase in adverse events such as skin irritation (38.8% vs 31.5%) compared with the placebo group.[14] The safety, efficacy, and benefits of NSAIDs are well outlined in the literature, and their use should be considered in the management of knee osteoarthritis.
Additional studies have assessed novel topical therapies, such as herbal remedies and capsaicin. Hedera helix, an evergreen ivy plant with anti-inflammatory properties, has recently been studied for its use in the management of knee osteoarthritis.[15] The effects of H. helix gel versus diclofenac versus placebo were compared in an RCT with 150 patients.[15] H. helix and diclofenac significantly reduced stiffness and assisted with physical function compared with the placebo (P < .05).[15] H. helix showed a higher reduction in pain and stiffness than diclofenac, but the results were not statistically significant.[15] Herbal remedies such as H. helix require further study to validate their use over NSAIDs in knee osteoarthritis.
Capsaicin, a neurotoxin found in chili peppers, works via destruction of primary afferent fibres, which leads to its analgesic effect.[16] A systematic review examined the effects of capsaicin on osteoarthritis in various joints.[17] The review included five RCTs, of which three were for knee osteoarthritis. Capsaicin was of only moderate efficacy in reducing knee pain up to 20 weeks, as analyzed by the visual analogue scale.[17] Although there was mild topical site burning and local skin irritation in 35% to 100% of patients, it was concluded that the treatment was safe and well tolerated and had no systematic effects.[17] However, further study is needed to assess the efficacy of capsaicin compared with the gold standard, topical treatment with NSAIDs.
The use of cannabis to manage osteoarthritis pain is being studied, but no clinical trials have been reported in the literature. A retrospective review of 71 patients who self-reported cannabis use in the perioperative period of total knee arthroplasty showed no improvement in total length of hospital stay, no reduction in in-hospital total morphine equivalent consumption, and no difference in postoperative functional outcomes up to 1 year after surgery.[18] Despite these results, given the ongoing opioid crisis in North America, investigation of alternative therapies for pain management in knee osteoarthritis is an essential area of focus for future research.
Steroid and hyaluronic acid injections
Corticosteroid injections have been used in osteoarthritis for their anti-inflammatory effects and ability to block the immune cascade, which results in reduced swelling and pain, and ultimately increased function.[19] Several studies have outlined the efficacy of steroid injections in reducing pain.[20-23] In an RCT in which 125 patients were randomly assigned to receive either prednisolone or a placebo, the prednisolone group had a statistically significant improvement in 6-minute walking distance, patient global assessment, knee pain, and benefits to physical function at 6 weeks compared with the placebo group (P < .05, P < .001, P < .001, and P < .05, respectively).[20] Additionally, there was a reduction in inflammatory markers such as Interleukin-1, Interleukin-5, tumor necrosis factor alpha, and high-sensitivity C-reactive protein in the treatment group compared with the placebo group, which persisted at both 6 and 12 weeks.[20] The use of corticosteroids was further validated in a prospective multicentre cohort study that examined the effects of intra-articular corticosteroid injections in knee osteoarthritis at 3 weeks, 6 weeks, 3 months, and 6 months.[21] All 100 participants had improved scores in the visual numeric scale and WOMAC at every time point except at 6 months for the visual numeric scale (P < .0001).[21] It was concluded that intra-articular corticosteroid injections are beneficial for pain and function and should, therefore, be considered in the management of knee osteoarthritis.[21] In an RCT involving 117 patients, the effects of an intra-articular corticosteroid injection were compared with those of a placebo using the visual analogue scale and WOMAC.[22] There was a statistically significant decrease in pain in the treatment group compared with the placebo group at 2 weeks and 6 weeks but not at 12 weeks, which indicated that corticosteroids were effective only in the short term.[22] A systematic review of 27 RCTs with a total of 1767 participants examined the efficacy and duration of intra-articular corticosteroid injections; however, it was unclear whether corticosteroid injections were significantly and clinically effective at reducing knee osteoarthritis pain after 1 to 6 weeks.[23] Additionally, the American Academy of Orthopaedic Surgeons has downgraded its recommendation regarding intra-articular steroid injections to moderate efficacy because studies have indicated that they may accelerate osteoarthritis through chondrotoxicity.[24,25] Although recent literature has called into question the long-term efficacy of corticosteroid injections, there remains substantial evidence that they are beneficial for short-term pain relief in knee osteoarthritis. There is no lifetime limit for the number of steroid injections in a particular joint.
Hyaluronic acid is a glycosaminoglycan that is considered to be a key element of cartilage and synovial fluid.[19] Inflammation occurs in knee osteoarthritis, which leads to alteration of the viscoelastic nature of synovial fluid and a reduction in the concentration and weight of hyaluronic acid.[19] Supplementation via intra-articular injection is thought to work by re-establishing the lubricating effect of the synovial fluid.[19] However, the literature is divided regarding the efficacy and benefits of viscosupplementation for pain reduction. A systematic review and meta-analysis of 89 studies with 12 667 patients showed no clinical benefit in terms of pain reduction associated with the use of hyaluronic acid.[26] In contrast, a meta-analysis of 54 trials and 7545 patients indicated that intra-articular hyaluronic acid had a therapeutic effect at 4, 8, and 24 weeks.[27] Cross-linked preparations tend to be more effective than older preparations; hence the variability in the literature. Viscosupplementation may have a role in the office setting, but currently, the American Academy of Orthopaedic Surgeons does not recommend routine usage of hyaluronic acid injections because of the lack of evidence showing clinically relevant differences associated with their use.[28] Some patients may benefit greatly from these injections, but they need to be counseled that not everyone benefits from them, and the cost is substantial. If the patient agrees to be treated, it is reasonable to offer one injection. If the patient benefits for at least 4 to 6 months, another injection can be given.
Stem cell injections
Intra-articular stem cell injection is an emerging novel therapy that is currently being investigated for its use in knee osteoarthritis. Mesenchymal stem cells have a complex mechanism of action and are thought to provide beneficial effects via their anticatabolic, anabolic, and anti-inflammatory mechanisms of action.[29] Mesenchymal stem cells are harvested from bone marrow and adipose tissue via minimally invasive approaches and can be injected into the intra-articular space.[29] Multiple studies on treating osteoarthritis with intra-articular injection of stem cells have demonstrated therapeutic effects in terms of pain management and functional benefits and have indicated that the treatment has no permanent adverse effects and is safe for use.[30-33] However, although the treatment could provide significant benefits to patients and prevent osteoarthritis disease progression,[30-33] the literature lacks robust data to support routine use of the treatment in clinical practice. Most studies have small sample sizes, there are concerns about the methodology used, and often the studies do not include a control group.[29] In addition, the cost of mesenchymal stem cell injections for osteoarthritis management is significantly higher than that of other therapies. As health systems develop economic awareness and continue to improve their cost-effectiveness, the use of mesenchymal stem cell injections is likely to fall by the wayside unless significant clinical benefit can be demonstrated in future well-designed studies.
Summary
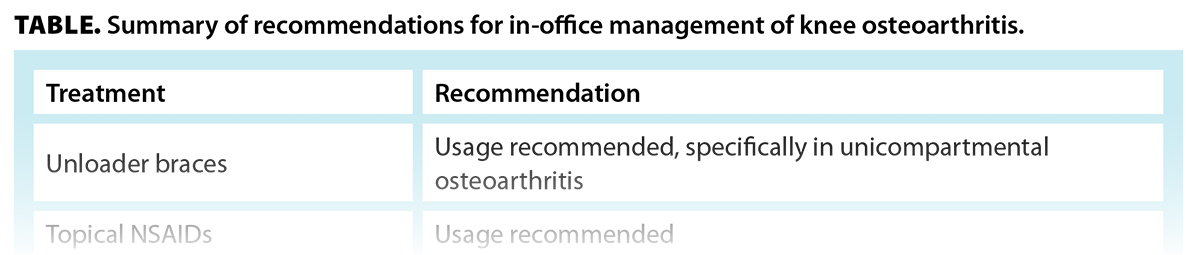
Osteoarthritis is becoming increasingly prevalent in Canada due to an aging population, and it has a significant economic impact. Nonsurgical management options should be used for knee osteoarthritis, either as temporizing measures while patients wait for a total knee arthroplasty or as definitive measures in less severe disease. With long surgical wait times, there is a need for conservative therapies to bridge and delay surgical intervention. Clinical therapeutic modalities such as unloader braces, topical treatments, and intra-articular steroids have been shown to be beneficial for both pain management and function in knee osteoarthritis. These modalities are summarized in the Table. Further research into the use of hyaluronic acid and mesenchymal stem cell injections is needed to warrant their routine use in the clinic setting.
Competing interests
None declared.
This article has been peer reviewed.
 |
| This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. |
References
1. Public Health Agency of Canada. Osteoarthritis in Canada: Highlights from the Canadian Chronic Disease Surveillance System. Last updated 24 December 2020. Accessed 7 August 2022. www.canada.ca/en/public-health/services/publications/diseases-conditions/osteoarthritis.html.
2. Public Health Agency of Canada. Chapter 6: Economic burden of arthritis. In: Life with arthritis in Canada: A personal and public health challenge. Last updated 19 July 2010. Accessed 7 August 2022. www.canada.ca/en/public-health/services/chronic-diseases/arthritis/life-arthritis-canada-a-personal-public-health-challenge/chapter-six-economic-burden-of-arthritis.html.
3. Sharma L. Osteoarthritis of the knee. N Engl J Med 2021;384:51-59.
4. Mistry DA, Chandratreya A, Lee PYF. An update on unloading knee braces in the treatment of unicompartmental knee osteoarthritis from the last 10 years: A literature review. Surg J (NY) 2018;4:e110-e118.
5. Brouwer RW, van Raaij TM, Verhaar JA, et al. Brace treatment for osteoarthritis of the knee: A prospective randomized multi-centre trial. Osteoarthritis Cartilage 2006;14:777-783.
6. Thoumie P, Marty M, Avouac B, et al. Effect of unloading brace treatment on pain and function in patients with symptomatic knee osteoarthritis: The ROTOR randomized clinical trial. Sci Rep 2018;8:10519.
7. Kirkley A, Webster-Bogaert S, Litchfield R, et al. The effect of bracing on varus gonarthrosis. J Bone Joint Surg Am 1999;81:539-548.
8. Lee PY, Winfield TG, Harris SR, et al. Unloading knee brace is a cost-effective method to bridge and delay surgery in unicompartmental knee arthritis. BMJ Open Sport Exerc Med 2017;2:e000195.
9. Moller F, Ortíz-Muñoz L, Irarrázaval S. Offloader knee braces for knee osteoarthritis. Medwave 2021;21:e8115.
10. Crofford LJ. Use of NSAIDs in treating patients with arthritis. Arthritis Res Ther 2013;15(Suppl 3):S2.
11. Baer PA, Thomas LM, Shainhouse Z. Treatment of osteoarthritis of the knee with a topical diclofenac solution: A randomised controlled, 6-week trial [ISRCTN53366886]. BMC Musculoskelet Disord 2005;6:44.
12. Conaghan PG, Dickson J, Bolten W, et al. A multicentre, randomized, placebo- and active-controlled trial comparing the efficacy and safety of topical ketoprofen in transfersome gel (IDEA-033) with ketoprofen-free vehicle (TDT 064) and oral celecoxib for knee pain associated with osteoarthritis. Rheumatology (Oxford) 2013;52:1303-1312.
13. Bookman AA, Williams KSA, Shainhouse JZ. Effect of a topical diclofenac solution for relieving symptoms of primary osteoarthritis of the knee: A randomized controlled trial. CMAJ 2004;171:333-338.
14. Wadsworth LT, Kent JD, Holt RJ. Efficacy and safety of diclofenac sodium 2% topical solution for osteoarthritis of the knee: A randomized, double-blind, vehicle-controlled, 4 week study. Curr Med Res Opin 2016;32:241-250.
15. Dehghan M, Saffari M, Rafieian-kopaei M, et al. Comparison of the effect of topical Hedera helix L. extract gel to diclofenac gel in the treatment of knee osteoarthritis. J Herb Med 2020;22:100350.
16. Guedes V, Castro JP, Brito I. Topical capsaicin for pain in osteoarthritis: A literature review. Reumatol Clín (Engl Ed) 2018;14:40-45.
17. Laslett LL, Jones G. Capsaicin for osteoarthritis pain. Prog Drug Res 2014;68:277-291.
18. Jennings JM, Angerame MR, Eschen CL, et al. Cannabis use does not affect outcomes after total knee arthroplasty. J Arthroplasty 2019;34:1667-1669.
19. Ayhan E, Kesmezacar H, Akgun I. Intraarticular injections (corticosteroid, hyaluronic acid, platelet rich plasma) for the knee osteoarthritis. World J Orthop 2014;5:351-361.
20. Abou-Raya A, Abou-Raya S, Khadrawi T, Helmii M. Effect of low-dose oral prednisolone on symptoms and systemic inflammation in older adults with moderate to severe knee osteoarthritis: A randomized placebo-controlled trial [retracted in: J Rheumatol 2018;45:1713]. J Rheumatol 2014;41:53-59.
21. Matzkin EG, Curry EJ, Kong Q, et al. Efficacy and treatment response of intra-articular corticosteroid injections in patients with symptomatic knee osteo-arthritis. J Am Acad Orthop Surg 2017;25:703-714.
22. Shrestha R, Shrestha R, Thapa S, et al. Clinical outcome following intra-articular triamcinolone injection in osteoarthritic knee at the community: A randomized double blind placebo controlled trial. Kathmandu Univ Med J 2018;16:175-180.
23. Jüni P, Hari R, Rutjes AW, et al. Intra-articular corticosteroid for knee osteoarthritis. Cochrane Database Syst Rev 2015;2015(10):CD005328.
24. Martin CL, Browne JA. Intra-articular corticosteroid injections for symptomatic knee osteoarthritis: What the orthopaedic provider needs to know. J Am Acad Orthop Surg 2019;27:e758-e766.
25. McAlindon TE, LaValley MP, Harvey WF, et al. Effect of intra-articular triamcinolone vs saline on knee cartilage volume and pain in patients with knee osteoarthritis: A randomized clinical trial. JAMA 2017;317:1967-1975.
26. Rutjes AWS, Jüni P, da Costa BR, et al. Viscosupplementation for osteoarthritis of the knee: A systematic review and meta-analysis. Ann Intern Med 2012;157:180-191.
27. Bannuru RR, Natov NS, Dasi UR, et al. Therapeutic trajectory following intra-articular hyaluronic acid injection in knee osteoarthritis—Meta-analysis. Osteoarthritis Cartilage 2011;19:611-619.
28. Brophy RH, Fillingham YA. AAOS clinical practice guideline summary: Management of osteoarthritis of the knee (nonarthroplasty), third edition. J Am Acad Orthop Surg 2022;30:e721-e729.
29. Lopa S, Colombini A, Moretti M, de Girolamo L. Injective mesenchymal stem cell-based treatments for knee osteoarthritis: From mechanisms of action to current clinical evidences. Knee Surg Sports Traumatol Arthrosc 2019;27:2003-2020.
30. Freitag J, Bates D, Wickham J, et al. Adipose-derived mesenchymal stem cell therapy in the treatment of knee osteoarthritis: A randomized controlled trial. Regen Med 2019;14:213-230.
31. Lee W-S, Kim HJ, Kim K-I, et al. Intra-articular injection of autologous adipose tissue-derived mesenchymal stem cells for the treatment of knee osteoarthritis: A phase IIb, randomized, placebo-controlled clinical trial. Stem Cells Transl Med 2019;8:504-511.
32. Zhao D, Pan J-K, Yang W-Y, et al. Intra-articular injections of platelet-rich plasma, adipose mesenchymal stem cells, and bone marrow mesenchymal stem cells associated with better outcomes than hyaluronic acid and saline in knee osteo-arthritis: A systematic review and network meta-analysis. Arthroscopy 2021;37:2298-2314.e10.
33. Jiang P, Mao L, Qiao L, et al. Efficacy and safety of mesenchymal stem cell injections for patients with osteoarthritis: A meta-analysis and review of RCTs. Arch Orthop Trauma Surg 2021;141:1241-1251.
Dr Sidhu is a resident in the Department of Orthopaedics, University of British Columbia. Dr Sheridan is a consultant orthopaedic surgeon at Gallway University Hospital, University of Gallway, Ireland. Dr Badii is a clinical assistant professor in the Division of Rheumatology, Faculty of Medicine, UBC. Dr Masri is a professor of orthopaedics at UBC and an orthopaedic surgeon at Vancouver General Hospital and UBC Hospital.
Corresponding author: Dr Bassam Masri, bas.masri@vch.ca.