Real-Time Virtual Support: Much-needed rural and remote assistance during the pandemic
The COVID-19 pandemic continues to impact rural and remote regions in Northern BC at a disproportionate rate compared with the rest of the province. More than 100 patients have had to be transferred out of Northern Health since the start of the fourth wave to hospitals with more ICU capacity. The vast majority of those have been COVID-positive. And with vaccination rates lower than in other areas of the province, a higher percentage of the population is at risk of getting critically ill from the fifth wave.
The impact on health care workers in a remote community like Chetwynd (population just over 3000) is far-reaching. The help being offered by Real-Time Virtual Support (RTVS) physicians, who are available 24/7 over Zoom, has been welcomed with open arms. And physicians are reporting that RTVS is having an impact on outcomes and helping alleviate the challenges of rural medicine during the pandemic.
RTVS virtual providers are physicians with experience in rural medicine and are dedicated to offering shoulder-to-shoulder support to physicians, residents, nurse practitioners, and nurses—any rural health care worker—over Zoom. The RTVS physicians, who are based throughout the province, can help with urgent and non-urgent cases and questions, including case consultations, second opinions, ongoing patient support, point-of-care ultrasound, and simulations.
When a critically ill patient cannot be managed at a rural site, RTVS physicians can also step in to coordinate their transfer to a larger centre through the Patient Transfer Network run by BC Emergency Health Services. The transfer is made to a centre with available ICU capacity. In recent months, due to critically ill COVID-19 patients, patient transfer has become more common.
Dr Bron Finkelstein, a new-to-practice doctor in Chetwynd, where the hospital has just five beds, says RTVS physicians have been instrumental in making stressful situations manageable with advice, guidance when a colleague is needed, and taking on patient transfers during the depths of a difficult situation. With RTVS support, the patient can be stabilized while a transfer is being arranged.
Dr Jodie Graham, chief of staff at Chetwynd Hospital, has trained and worked in rural medicine for over a decade, including in rural Alberta, the Northwest Territories, and Yukon, and agrees that RTVS is the best thing to happen to rural medicine.
Dr Matt Petrie is an RTVS physician who has helped coordinate patient transfers for the Chetwynd team, pointing out that it is sometimes difficult for doctors in urban centres to understand the situation on the ground in a rural centre. As a member of the RUDi (emergency) team in RTVS, he understands that part of his job is to advocate for rural providers who may not be able to advocate for themselves and their community during a stressful situation.
Call early and call often
Dr Finkelstein urges health care providers to call RTVS early—before they get too busy to call—and to call often—when they have a significant case, a challenging case, a case where a second opinion would be beneficial. He’s never encountered someone who was unwilling or unhappy to talk. Providers throughout the province are encouraged to reach out for support.
For more information on how to get started with RTVS, visit https://rccbc.ca/rtvs/getting-started.
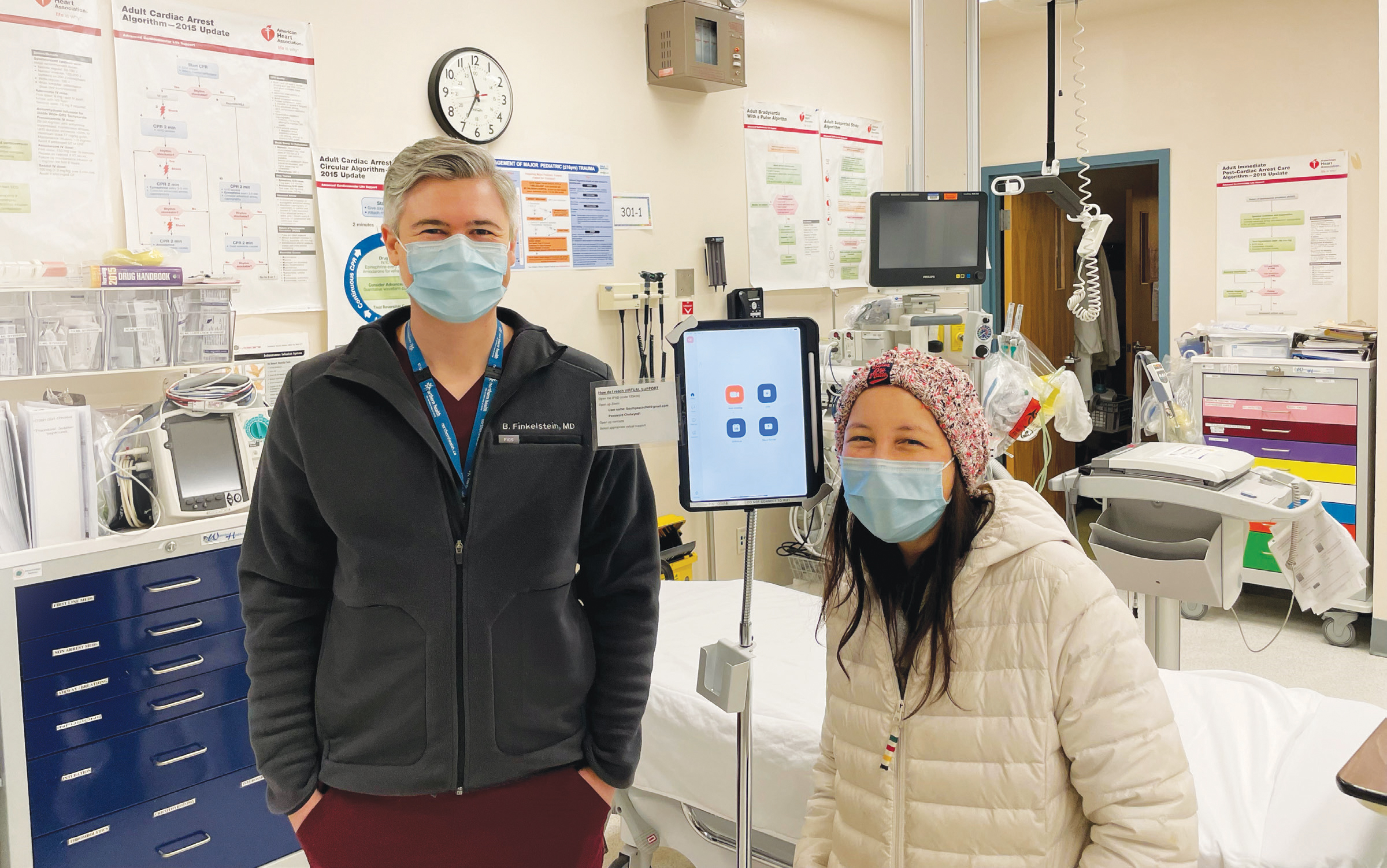
Drs Bron Finkelstein (left) and Jodie Graham (right), from Chetwynd, are frequent users of the Real-Time Virtual Support pathways for providers.
hidden
 |
| This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. |
