Clinical Images
A case of eumycetoma in British Columbia
Although eumycetoma is a rare infectious entity in Canada, its diagnosis should be considered in patients who have arrived from an endemic country.
Eumycetoma is a rare, chronic disease in which fungal entities implant into various body tissues, causing granulation and inflammation.[1] It is endemic in countries along the tropics and affects approximately 1.81 people per 100 000.[2] The fungal agent may initially cause local inflammation and swelling; over a chronic course, it invades subcutaneous tissues. If untreated, this may result in irreversible derangements to soft tissue structure and debilitating injury. Due to the paucity of guidelines, diagnosis and management of this rare entity remain uncertain.
We present the case of a 23-year-old female immigrant from Somalia who had an enlarging knee mass since childhood. Soft-tissue sarcoma was the initial preliminary diagnosis. MRI with sagittal T2 gradient-recalled echo and axial T1 fat-saturated acquisitions demonstrated a mildly lobulated 2.36 × 5.32 × 8.64 cm heterogeneous but predominantly T1/T2 hyperintense mass, along with mild peripheral susceptibility artifact and mild surrounding inflammatory change [Figure 1]. It contained multiple septations and foci of hypointense debris, suggestive of edema or necrosis.
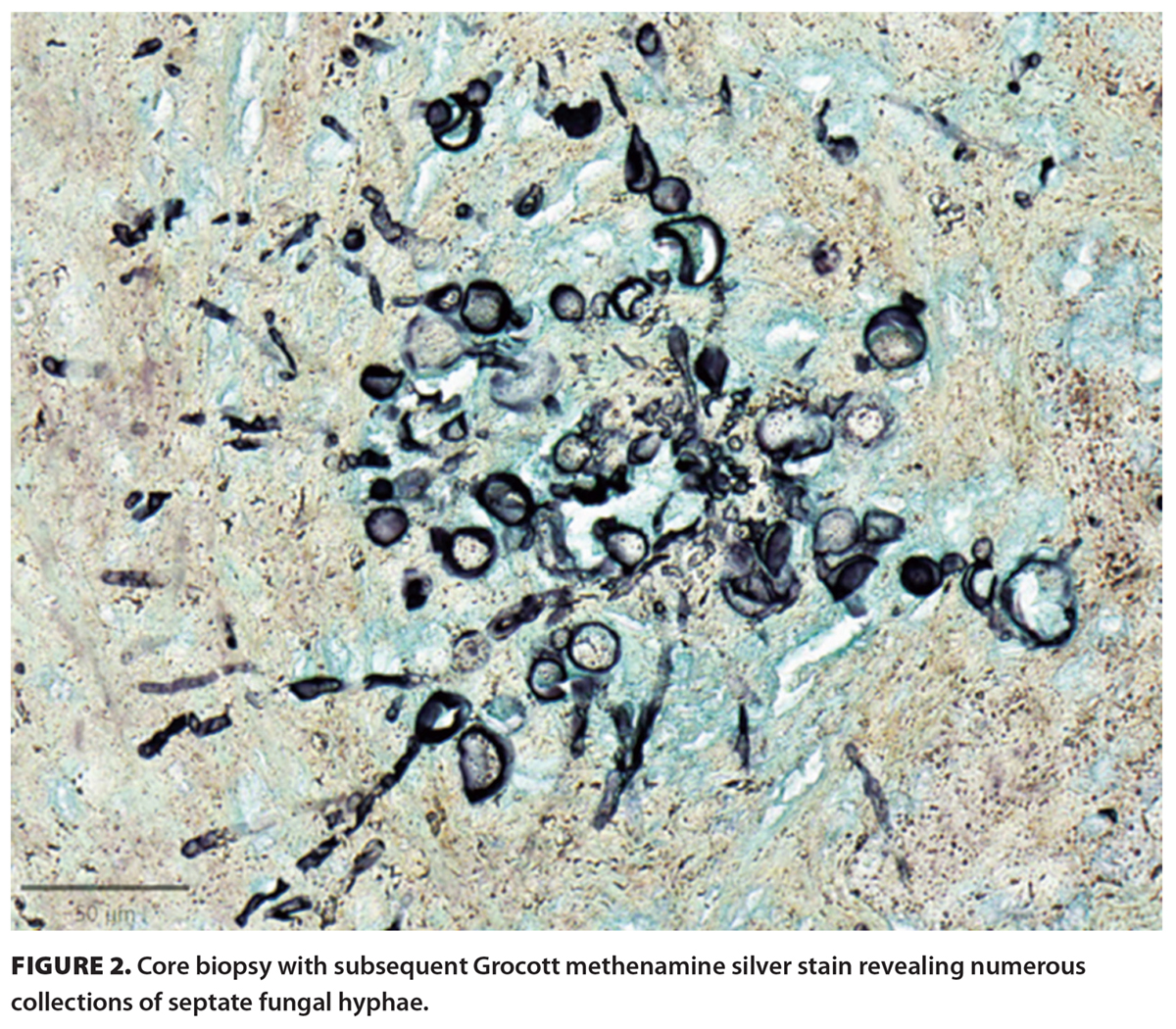
The patient underwent surgical removal of the mass and had symptomatic improvement. Subsequent core biopsy with Grocott staining revealed a dense collection of fungal elements with surrounding inflammation and edema [Figure 2]. There were various collections of septate fungal hyphae surrounded by the Splendore–Hoeppli phenomenon, consistent with a eumycetoma. No specific organisms could be recognized. After a few weeks of culture, no fungal or bacterial elements were isolated.
This unique case highlights a few points. Eumycetoma, a rare infectious entity in Canada, should be on the differential for patients who have arrived from an endemic country. Infection may include soft tissue entities, such as lipoma, sarcoma, or neuroma. Treatment is patient-dependent and, depending on the clinical scenario, involves observation, treatment with antifungal agents, or surgical resection.[3] With the number of immigrants increasing due to global mobilization, practitioners should include atypical infectious causes in the differential diagnosis, which will aid in accurate diagnosis and timely management.
Acknowledgments
The authors greatly appreciate Dr Sanjiv K. Bhalla’s contributions to the MRI image interpretation.
Competing interests
None declared.
hidden
This article has been peer reviewed.
 |
| This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. |
References
1. Chandler DJ, Bonifaz A, van de Sande WWJ. An update on the development of novel antifungal agents for eumycetoma. Front Pharmacol 2023;14:1165273.
2. Emery D, Denning DW. The global distribution of actinomycetoma and eumycetoma. PLoS Negl Trop Dis 2020;14:e0008397.
3. Hao X, Cognetti M, Burch-Smith R, et al. Mycetoma: Development of diagnosis and treatment. J Fungi 2022;8:743.
hidden
Dr Chen was a medical student at the University of British Columbia at the time of article submission. He is currently a resident physician at McGill University. Dr Mirzanejad is a clinical professor in the Division of Infectious Diseases at UBC, an infectious diseases consultant at the Surrey Memorial Hospital Campus and Jim Pattison Outpatient Centre, chair of the Tropical Medicine Expert Group of BC, and clinical lead for undergraduate education, UBC, at the Surrey site.