HPV vaccine revolutionizes prevention of cervical cancer
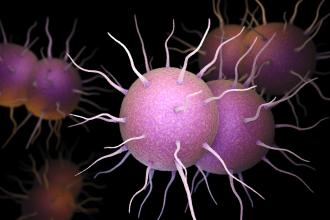
Cervical cancer is the second most common cancer in women worldwide. Human papillomavirus (HPV) causes cancer of the cervix. HPV is the most common sexually transmitted infection (STI) and 8 of 10 adults will become infected; 9 of 10 infected women will clear the virus but the rest may develop persistent infection and progressive neoplasia.
HPV vaccines prevent infection. British Columbia will start offering HPV vaccine to girls in grades 6 and 9 in school-based clinics in the fall of 2008.
Tertiary prevention
A patient I met as a clinical clerk on gynecology 25 years ago was a married woman with two small children in her late twenties. During her second pregnancy she was diagnosed with cancer of the cervix.
Postpartum she had an inadequate course of treatment. The pelvic exenteration involved radical pelvic resection of a mass and surrounding tissue followed by reconstructive surgery to recreate a vagina using muscle flaps from the inner thigh.
Secondary prevention
The Pap smear identifies curable precancerous cervical abnormalities. Each year in BC over half a million women get a Pap smear, and over 5000 are treated for cervical intraepithelial neoplasm 2 and 3.
This program has reduced the incidence and mortality from cervical cancer by about 70%. Pap smears save lives. But each year in BC about 40 to 50 women die from invasive cervical cancer and 100 women are newly diagnosed with cervical cancer due to HPV types 16 or 18. Most deaths occur in unscreened or under-screened women.
Primary prevention
There are now two vaccines designed to prevent cancer of the cervix, Gardasil (Merck Frosst) and Cervarix (GlaxoSmithKline). Gardasil was approved in Canada for girls and women aged 9 to 26 years in July 2006 and is now approved in over 100 countries. It is a quadrivalent vaccine against HPV types 6, 11, 16, and 18. Cervarix has type 16 and 18 protection and is not yet approved in Canada.
Worldwide, HPV types 16 and 18 account for 70% of cervical cancer; types 6 and 11 cause 90% of genital warts. In clinical trials in young women, both vaccines demonstrated high efficacy in preventing pre-neoplastic cervical abnormalities. Both are immunogenic in adolescents.
Gardasil is recommended by the National Advisory Committee on Immunization for girls aged 9 to 13 years as this is an age prior to sexual activity.[1] However, even sexually active girls and women are unlikely to have acquired infection with both oncogenic HPV types and can benefit from immunization.
Immunized women still need regular Pap tests until we know how vaccination will affect screening programs. The vaccines are not approved for use in males at this time as results from clinical trials are pending.
Gardasil is given in three doses over 6 months (at 0, 2, and 6 months). Studies are ongoing to establish duration of protection but currently indicate a minimum of 5 years.[2] Mathematical modeling of HPV 16 antibody decay suggests that about three-quarters of immunized women may have lifelong protection.[3]
Gardasil is safe and well tolerated in clinical trials and postmarketing use.[4] Over 20 million doses have been distributed worldwide. Local injection site reactions include pain, redness, and swelling. In clinical trials, systemic adverse events like headache or fatigue were as common in placebo as in vaccine recipients. Fainting has been reported both before and after the vaccine in school-based clinics and a short period of observation postvaccination is recommended.
Media coverage of these vaccines indicates some misconceptions. A national survey done before the summer of 2007 found that 74% of parents intended to vaccinate their daughters; 63% in BC.[5] The family doctor will influence the decision for many girls, parents, and young women.
Information will be going home with grade 5 and 8 girls at the end of term in advance of the autumn program. HPV vaccines do not prevent pregnancy or other STIs. HPV vaccines do not cause young girls to have sex. But these vaccines will prevent cervical cancer. Physicians should be prepared to tell the facts.
For updates, check our web site periodically at www.bccdc.org.
—Monika Naus, MD, MHSc
References
1. National Advisory Committee on Immunization. Statement on Human Papillomavirus Vaccine. Can Communic Dis Rep 15 Feb 2007;33(ACS-2):1-32. www.phac-aspc.gc.ca/publicat/ccdr-rmtc/07vol33/acs-02/index_e.html (accessed 1 May 2008).
2. Villa LL, Costa RL, Petta CA, et al. High sustained efficacy of a prophylactic quadrivalent human papillomavirus types 6/11/16/18 L1 virus-like particle vaccine through 5 years of follow-up. Br J Cancer 2006;95:1459-1466.
3. Fraser C, Tomassini JE, Xi L, et al. Modeling the long-term antibody response of a human papillomavirus like particle type 16 prophylactic vaccine. Vaccine 2007;25:4324-4333.
4. Gardasil Product Monograph. Merck Frosst Canada Ltd. www.merckfrosst.com/mfd/en/corporte/products/gardasil.html (accessed 10 May 2008).
5. Ogilvie GS, Remple VP, Marra F, et al. Parental intention to have daughters receive the human papillomavirus vaccine. CMAJ 2007;177:1506-1512.