Syphilis: Shifting trends in BC and new tools for clinical practice
Syphilis, caused by the spirochete Treponema pallidum, is a sexually transmitted infection that can lead to significant adverse outcomes across organ systems if left untreated.[1] Syphilis has a well-earned reputation as “the great imitator,” as it can impact any organ system and present in a variety of ways. Because no immunity develops, reinfection after treatment is a risk with subsequent exposures. Infectious syphilis is usually categorized into primary, secondary, and early latent syphilis. Late latent syphilis is considered non-infectious. In BC, there is a stage called latent syphilis of unknown duration, which may or may not be infectious. Vertical transmission during pregnancy or delivery can result in miscarriage, stillbirth, or congenital syphilis, which poses significant health risks to infants.[1]
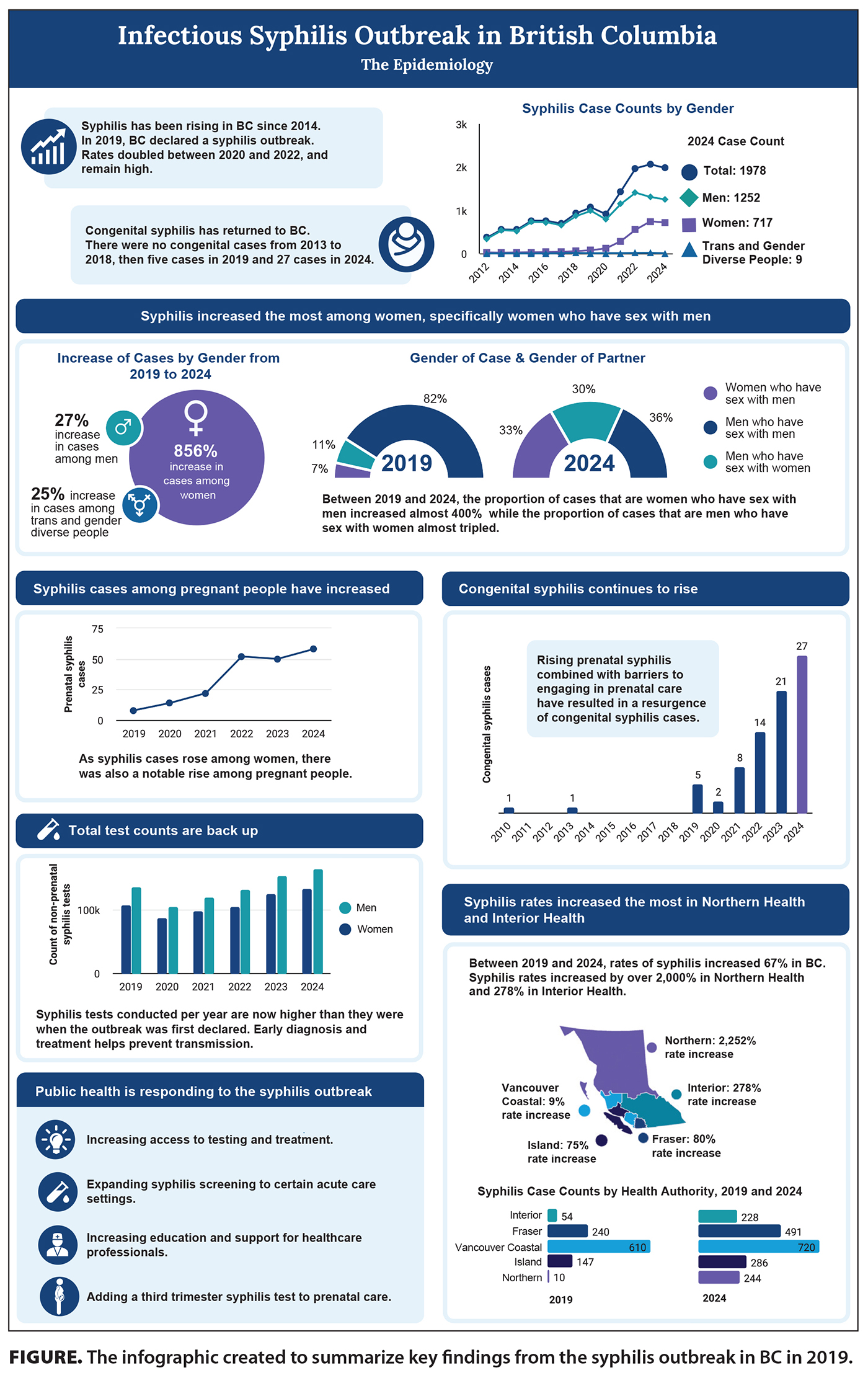
British Columbia declared a syphilis outbreak in 2019 following a sharp rise in cases and the re-emergence of congenital syphilis.[2] Given the current outbreak and change in epidemiology, we encourage clinicians to think about syphilis and offer testing. For comparison, in 2010 (pre-outbreak), the rate of infectious syphilis was 3.4 per 100 000.[3] By 2019, this had increased to 20.9 per 100 000. In 2023, the rate peaked at 37.5 per 100 000. Rates have been stable since 2025 but remain high compared with pre-outbreak levels.[3]
Historically, gay, bisexual, and other men who have sex with men accounted for most reported cases. However, a notable shift in the epidemiology occurred during the outbreak toward rising rates among heterosexual populations, particularly women, and increased incidence among individuals experiencing unstable housing and substance use. Between 2019 and 2024, syphilis rates also rose significantly in regions outside major urban centres, with the Northern Health Authority experiencing a rate increase of over 2000% and the Interior Health Authority seeing a 278% rise.[3,4] While smaller population sizes amplify rate changes, the geographic expansion of cases into more rural and remote areas signals an important trend for health professionals to be aware of. A notable rise among pregnancies complicated by syphilis has seen the return of congenital syphilis, a previously rare occurrence, with no congenital cases reported in the province from 2013 to 2018. In 2019, five congenital syphilis cases were identified, with case counts increasing annually to 27 cases in 2024. An additional 11 congenital syphilis cases were reported in the first two quarters of 2025.[3,4] Updated screening recommendations have been implemented for pregnant individuals to be screened twice in the perinatal period: the first in the first trimester or at the first prenatal visit, and the second at delivery or anytime after 35 weeks for home births.
 We have developed new communication tools to help busy clinicians stay aware of the changing trends; to help clinicians think about and test for syphilis, including swabbing lesions; to assist with serology; and to help clients understand disease risk, prevention, and treatment options. These tools include:
We have developed new communication tools to help busy clinicians stay aware of the changing trends; to help clinicians think about and test for syphilis, including swabbing lesions; to assist with serology; and to help clients understand disease risk, prevention, and treatment options. These tools include:
- An infographic. Traditional surveillance resources, such as the new interactive Sexually Transmitted and Blood Borne Infection (STBBI) and Tuberculosis (TB) Surveillance Report[4] and key trend reports,[5] offer comprehensive data but may not clearly highlight emerging trends for busy clinicians. To address this, a concise and visually accessible infographic was created to summarize key findings from the outbreak [Figure].
- A tool kit for health professionals. Complementing the infographic is a tool kit, which includes:
- A quick-reference handbook for recognizing clinical presentations and testing methods.
- Serology interpretation guides.
- Patient education materials.
To download the infographic and tool kit, including posters and patient education materials, visit www.bccdc.ca/health-professionals/clinical-resources/syphilis-toolkit.
Anyone who is sexually active can get syphilis. Clinicians are encouraged to consider syphilis screening for patients with sociodemographic risk factors, including unstable housing and substance use, and add syphilis blood work to routine screening for sexually transmitted infections. For symptomatic presentations, ensure lesions are swabbed along with submitting blood work to aid in infection staging. Sample requisitions and reference tools for specimen collection are available in the tool kit for health professionals. For assistance with syphilis case management or follow-up, contact the BCCDC public health nurse at 604 707-5607 or physician at 604 707-5610. To request a digital copy of the Syphilis Handbook or a printed version of the full tool kit, email sticourse@bccdc.ca.
—Julie Holt, RN, MHM
Senior Practice Leader, Communicable Disease Prevention and Response, BCCDC
—Hannah M. Baer, PhD
Epidemiologist, Communicable Disease Prevention and Response, BCCDC
—Kirsty Bobrow, MBChB, DPhil, MSc
Medical Director, Communicable Disease Prevention and Response, BCCDC
—Barbra Arnold, MD, CCFP
Physician, Communicable Disease Prevention and Response, BCCDC
—Rochelle Stimpson, MD, CCFP
Physician, Communicable Disease Prevention and Response, BCCDC
hidden
This article is the opinion of the BC Centre for Disease Control and has not been peer reviewed by the BCMJ Editorial Board.
 |
| This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. |
References
1. Tudor ME, Al Aboud AM, Leslie SW, Gossman W. Syphilis. Statpearls [Internet]. Updated 17 August 2024. Accessed 22 August 2025. Treasure Island, FL: StatPearls Publishing; 2025. www.ncbi.nlm.nih.gov/books/NBK534780/.
2. BC Centre for Disease Control. BC syphilis action plan refresh, 2023–2025. March 2023. Accessed 3 October 2025. www.bccdc.ca/resource-gallery/Documents/Statistics%20and%20Research/Statistics%20and%20Reports/STI/Syphilis_Action_Plan_Refresh_2023.pdf.
3. BC Centre for Disease Control. Syphilis indicators in British Columbia: BCCDC CPS surveillance report. 2025. Accessed 3 October 2025. www.bccdc.ca/resource-gallery/Documents/Statistics%20and%20Research/Statistics%20and%20Reports/STI/BCCDC_website_syphilis_indicators_2025Q2.pdf.
4. BC Centre for Disease Control. Sexually transmitted and blood borne infection (STBBI) and tuberculosis (TB) surveillance report. Accessed 3 October 2025. https://bccdc.shinyapps.io/stbbi_tb_surveillance_report.
5. BC Centre for Disease Control. STI reports. Accessed 3 October 2025. www.bccdc.ca/health-professionals/data-reports/sti-reports.

