Quarantine, tuberculosis, and the curtailment of freedom
My experience with curtailment of freedom as a quarantined tuberculosis patient in the 1950s is interesting to reflect upon at this time of COVID-19.
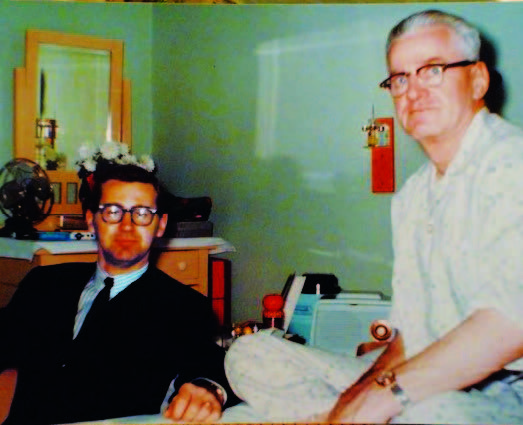 |
| A newly minted physician, Dr Zacharias returns to visit his father at the Ninette Sanatorium in southwestern Manitoba. |
The summer of 1956 began like any other. I had graduated from high school and was eager to face the world, focused on the promised land of a career in medicine. I began my summer vacation as an orderly at the King George Hospital in Winnipeg. The first week was spent getting acquainted with the hospital routine. I looked forward to going home to Winkler on the weekend.
Just as I arrived home, our family doctor called, wanting to see me. His first remark, “You have been burning the candle at both ends,” was a prelude to the reason for my visit home. A pre-employment chest X-ray had shown a shadow the size of a dime in the apex of my right lung. He suggested that I see a Dr Scott at the Central Tuberculosis Clinic (CTC) in Winnipeg on the following Monday morning, where my immediate future would be decided.
Disrupted plans
I arrived at the CTC on 15 July 1956 and had my first glimpse of the small X-ray shadow that was about to disrupt my previous plans. After brief deliberation, I was directed to spend 6 months in a TB sanatorium, under quarantine. I felt both surprise and disbelief. “You must be kidding! I feel perfectly well, and besides, I’m starting college in 2 months. You can’t do this to me!” I quickly learned that he could, and he would. By that evening, I had taken up residence at my new hospital address, the CTC in Winnipeg for 3 weeks, before moving on to the Ninette Sanatorium in southwestern Manitoba.
My roommates proved to be a pleasant group, but they were not very encouraging. The standard question around the place was, “How long did the doc say that you would be here?” My 6-month sentence drew laughter. One patient said, “Six months, eh. Don’t bet on it. You’ll be here for 2 years at least. I’m in for the third time. My last session lasted 5 years!” The next 3 weeks were the longest of my life. Imagine spending 23 hours a day in bed, even though you feel perfectly well. To make matters worse, the nurses’ tennis court was directly across the street! Never had I wanted to play tennis as much as I did during those 3 weeks spent in what I called “Cell 41.”
Families divided
The sanatorium at Ninette, the San for short, is located on a beautiful hillside overlooking Pelican Lake, 200 km west of Winnipeg. I joined my father there, as he had already been there 6 years. Father and son, together again, but in isolation! He had been forced, by contracting TB himself, to leave our family farm in 1950, at the age of 33, leaving behind a wife and five children, ranging in age from 1 to 12. I was the oldest. During those 6 years in hospital, he had undergone extensive “lung collapse therapy.” This included repeated pneumothoraces, plombage (Ping-Pong balls), wax packs, and at least three separate thoracoplasties, which involved the removal of multiple ribs. The end result was a loss of two-thirds of his lung capacity and severe shortness of breath at rest. All of these procedures were performed under local anesthetic.
My father’s departure from the farm had a major impact on my family. How was my mother to provide an income sufficient to raise five children? There was no social security income. The only answer was to continue farming. My younger brother and I worked on the farm until high school graduation, with the help of an uncle. This meant dawn-till-dusk days of physical work and included driving the tractor for planting, hoeing, and harvesting. We always needed time off school in spring and fall.
Tragedy again struck with the death of my mother. She died from an aggressive form of ovarian cancer when she was only 46. This was during my second year at the San, and my dad’s seventh year there. We were both given compassionate leave to return home for a brief time, but with strict precautions. Following this, we returned to Ninette and stayed there until the health authorities would declare us “safe to resume public life.” My cure, via triple therapy, would eventually take 2 years. My father, who was gaunt and quite underweight in 1950, missed out on triple therapy. He was hospitalized for 11 years in total. Sadly, he eventually died from TB and its complications. My dad had two brothers who developed TB, and they were both quarantined, far from home. Just like ours was, their families were greatly disrupted by their illnesses.
Chasing the cure
I became acquainted with the phrase, “to chase the cure.” This described the adjustment we all had to make. A brief idea of a day in the life of a TB crock: breakfast was served at 7:30. Dessert consisted of a handful of pills, para-aminosalicylic acid and isoniazid, nine at each meal. As a rookie I had some difficulty swallowing them one at a time, but after several weeks this became a one-shot affair. Streptomycin was given by injection twice per week, in the strep room. We queued up, and when we reached the front of the long line, we quickly bared our bottoms. This was before the days of disposable needles. The most important point was to learn to relax the gluteus maximus! Much of the day was spent in bed, and ingestion of the pills was strictly monitored.
After my first 3-week interval of triple therapy at Ninette, various tests and X-rays were taken in anticipation of conference day, or “judgment day.” The San medical staff presided. Upon entering the conference room, I was met by a long row of X-rays, the length depending on whether you were a veteran or a freshman. I was seated in a chair in the centre of the room, surrounded by the medical staff. My history was reviewed and discussed, and my X-rays were examined. While the men in the long white coats conversed in a language foreign to me, I’m sure my pulse rate hit 150 and I noticed that my hands were cold and clammy. Finally, my judgment was delivered. “Eighteen months if all goes well, and surgery may have to be considered.”
Increasing freedoms
As soon as my length of stay was determined, the capable rehabilitation division of the San moved in. I quickly realized that I might go mad if I had nothing to do. The University of Manitoba initially turned me down in my application to study first-year arts courses by correspondence, but they eventually let me in. I was their first student-patient studying by correspondence. My classes included English (studying Milton, Donne, and Chaucer), the history of Tudor England, economics, psychology, and sociology. There are many challenges when you are trying to learn without a teacher, this being long before the Internet. Through hard work and a fair measure of luck, I was able to get the Winnipeg professors to give me the nod, and I completed my first year of undergraduate study at the San.
 |
| After initially refusing his request, the University of Manitoba eventually let Dr Zacharias become their first student-patient to study by correspondence. |
After several months in the infirmary, one was gradually allowed certain freedoms and life became less dull. Male and female patients were housed in separate pavilions, but this did not stop secret communication between the sexes. I was particularly attracted to a lovely young lady who was dressed in a colorful, striped Hudson Bay coat. Christmas was celebrated with a large banquet held on Christmas Eve. The healthier crocks, now noninfectious, formed a choir, and in this way brought favorite carols to the less fortunate brothers and sisters who were confined to bed. The highlight of the festivities was a concert held a short time after Christmas. The staff and patients worked together to produce skits and musical numbers. The orchestra consisted of guitars and drums played by Indigenous patients, who were primarily Métis and Inuit. The program included their favorite western songs. Of interest was the absence of musical stands. The musicians preferred to have their sheet music spread out on the floor. I had the opportunity to direct a mixed Inuit choir, composed of 17 singers, who performed carols in Inuktut. A few dances added excitement to the program.
My roommates (up to 10 per room, coughing at night) and friends were a diverse group of World War II veterans, Indigenous people, and patients who had survived the brutal Hong Kong prison camps. The months progressed. Old friends were discharged and new ones arrived. Many of the chronic patients died from their disease. I became aware of the many social problems that came out of San life. Long periods of spousal separation often led to divorce, for example. An occasional friend, son, daughter, mom, or dad would not return from the OR. Moms and dads were helpless and suffered the anguish of their isolation from their loved ones back at home. The younger patients faced a future of uncertainty, while their friends were pursuing their dreams and goals in life.
Free at last
Twenty-three months after my arrival, the news of my discharge came, yet it caused little excitement. The San had become home to me, and friends outside its walls were almost strangers. I had some deep-seated fears: for my future health, of facing the outside world again, and that my friends would no longer understand or accept me.
Finally, on emancipation day, and carrying a tennis ball can full of pills (to be taken after discharge), sporting a clear chest X-ray, I departed from Ninette. I was grateful that the University of Manitoba awarded me an annual bursary of $700, which was contingent on my being accepted into, and surviving, medical school. After this eventful medical detour, my goal—to enter the promised land of medicine—would indeed come true.
Public health principles stand the test of time
During this COVID-19 pandemic, it is interesting to reflect that the key to controlling tuberculosis was free health care for those affected, contact tracing, and enforced isolation, all of which reduced the death rate in North America by 80% before the advent of streptomycin. Application of public health principles is just as critical today. Canada and the United States have used strikingly different approaches to COVID-19 containment and management. In some US states, individual rights and freedoms are trumping any enforcement for the public good, despite the soaring death rate resulting from those freedoms. There is a high price to be paid for allowing individual freedom to have priority over protecting the public. In Canada, the acceptance of isolation and social distancing is much greater, for the sake of protecting everyone.
Acknowledgments
Dr Zacharias thanks Drs Murray Woods and Giles Stevenson for their assistance with the preparation of this article.
hidden
This article has been peer reviewed.
hidden
Dr Zacharias is a retired radiologist living in Victoria. He is married to the “lady who was dressed in a colorful, striped Hudson Bay coat” whom he first met at the Ninette Sanatorium.



Thank you for sharing your experience I was sorry to hear of your families struggles and great losses with tb but grateful to hear your lengthy treatment was eventually effective. Your positive attitude, hard work and tenacity is inspiring
Wishing you and your lovely lady in the colorful coat continued health and happiness.