When hypotransferrinemia obscures the diagnosis of hereditary hemochromatosis: A case report
By impairing erythropoiesis, hypotransferrinemia may cause anemia. Hypotransferrinemia may also be a rare cause of iron overload. Another common cause of iron overload is C282Y homozygous hemochromatosis. While it is unusual to find the two disorders in the same patient, in this case, a 53-year-old male was found to have both conditions.
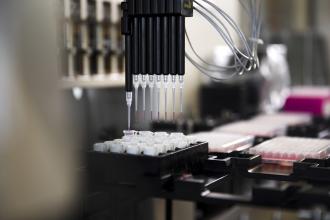
A patient with an iron overload disorder benefits from genetic testing that has become more readily available in BC.
A thin 53-year-old white male who had been diagnosed with hypotransferrinemia 5 years previously presented for reinvestigation of iron overload. At the time that the patient’s hypotransferrinemia was initially documented, he had a ferritin level of 465 µg/L (normal 15–250 µg/L). His transferrin level was 1.91 g/L (normal 2.20–3.80 g/L), and total iron-binding capacity (TIBC) was reduced at 39 µmol/L (normal 45–73 µmol/L), in concert with the hypotransferrinemia. He had borderline anemia and his major complaint was fatigue.
It was felt at the time of his initial diagnosis that the patient might have an undiagnosed “chronic disease” as well, but hemochromatosis was not considered because his transferrin saturation (TS) was too low at 79%. He was advised to donate blood and to decrease vitamin C and iron intake.
With advances in the understanding of iron overload it was decided to reinvestigate the patient 5 years after the initial diagnosis of hypotransferrinemia. At this time he was still complaining of unremitting fatigue. On examination the patient displayed a grayish-yellow discoloration of the skin. There was no palpable liver or stigmata of chronic liver disease. His blood pressure was normal. An ultrasound image of his liver showed a slightly enlarged organ but no other abnormalities. A different laboratory with differing standards was used in the follow-up evaluation. The patient’s ferritin level was 623 µg/L and his liver function tests were normal. He had a slightly elevated cholesterol level at 5.6 mmol/L (normal 2.0–5.2 mmol/L). His renal function, thyroid function, fasting blood sugar level, complete blood count, serum ceruloplasmin, and copper levels were all normal. Total iron was elevated at 32 µmol/L (normal 9–30 µmol/L) and TIBC was reduced at 41 (normal 45–70 µmol/L). The TS was 78% (normal 15%–55%). The elevation of the TS was partly explained by the low TIBC, as the TS was calculated using the total iron and TIBC.
Consideration was then given to the possibility of the patient having type 4 hemochromatosis or ferroportin disease because of the previous borderline anemia, high ferritin value, possible spuriously elevated TS, and no evidence of dysmetabolic hepatosiderosis. Ferroportin disease presents with a variable clinical phenotype. Transferrin saturation may be normal or elevated, ferritin level is elevated, and venesection therapy is often complicated by the development of anemia.[1] Type 1 or HFE hemochromatosis is the most common form of hemochromatosis.[2] Because of the increased availability of HFE gene testing for first-line genetic investigation of iron overload, the decision was made to test for this disorder before any testing for ferroportin disease was initiated.
HFE gene testing subsequently revealed the patient to be a C282Y homozygote. He then underwent venesection for the removal of 12 units of blood (equivalent to 3 g of iron) over 14 months until his ferritin level reached 66 µg/L. The iron reduction was deliberately prolonged as venesection therapy tended to precipitate red blood cell, hemoglobin, and hematocrit values below the normal range. After iron reduction, the patient’s fatigue did not improve and he complained of balding. However, his complexion assumed a more normal hue and a follow-up ultrasound image of the liver was normal.
Hypotransferrinemia is a relatively rare condition and is held to be autosomal recessive.[3-5] In hypotransferrinemia the transferrin deficiency causes dietary nontransferrin-bound iron to be deposited in the liver via the portal circulation.[6] Impaired erythropoiesis can also occur due to the decreased availability of transferrin to transport iron to erythrocytes, and anemia may result.
It is possible that in this case the concomitant C282Y homozygosity mitigated the tendency to anemia in the patient. The patient’s balding was likely due to a combination of genetic predisposition and the recurrent borderline anemia produced by venesection therapy. Paradoxically, in C282Y homozygous hemochromatosis body hair loss correlates with markedly increased iron stores and is related to hypogonadism.
Hypotransferrinemia is a rare disorder, but it may be more common than is clinically diagnosed and may complicate the diagnosis of patients with anemia and other coexisting disorders. This can be seen in the case reported here, where a 53-year-old male who had been diagnosed with hypotransferrinemia 5 years earlier presented with iron overload. The availability of HFE gene testing made it possible to consider coexisting hereditary hemochromatosis. The patient tested positive for two copies of the C282Y mutation and was then treated for coexisting hypotransferrinemia and C282Y homozygous hemochromatosis.
Competing interests
None declared.
References
1. Pietrangelo A. The ferroportin disease. Blood Cells Mol Dis 2004;32:131-138. PubMed Abstract Full Text
2. Feder JN, Gnirke A, Thomas W, et al. A novel MHC class I-like gene is mutated in patients with hereditary haemochromatosis. Nat Genet 1996;13:399-408. PubMed Abstract Full Text
3. Knisely AS, Gelbart T, Beutler E. Molecular characterization of a third case of human atransferrinemia. Blood 2004;104:2607. PubMed Citation Full Text
4. Beutler E, Gelbart T, Lee P, et al. Molecular characterization of a case of atransferrinemia. Blood 2000;96:4071-4074. PubMed Abstract Full Text
5. Stavem P, Saltvedt E, Elgjo K, et al. Congenital hypochromic microcytic anaemia with iron overload of the liver and hyperferraemia. Scand J Haematol 1973;10:153-160. PubMed Citation
6. Ponka P. Rare causes of hereditary iron overload. Semin Hematol 2002;39:249-262. PubMed Abstract
Chris Whittington, MB BS, MBA, FCFP, FACRRM
Dr Whittington is a clinical associate professor of family practice at the University of British Columbia and a staff member at MSA General Hospital, Abbotsford, British Columbia.