What can genomics do for health care?
Clinicians in BC today have a unique opportunity to advance patient care. With the recent support of the BC Clinical Genomics Network (BCCGN) by the Michael Smith Foundation for Health Research, physicians are now able to participate actively in research and at the same time improve patient care. The BC Clinical Genomics Network assists clinicians to carry out research studies on unique families and patient populations by providing access to state-of-the-art genomic technologies, assistance with genetic study design and analysis, and advice regarding patient consent and ethics. We describe a case report as an example in which the genomic technology single nucleotide polymorphism genotyping was used to look for common variations that were linked to a disease-causing mutation in a family of affected males. This article explains how this technology works and how it can be used in research to help patients and their families.
New genotyping technology is being used in BC to expand our understanding of the human genome and help address clinical problems.
Clinicians in BC today have a unique opportunity to advance patient care. Thanks to the Michael Smith Foundation for Health Research, which supports the British Columbia Clinical Genomics Network (BCCGN), physicians are now able to participate actively in extending the boundaries of knowledge and improving patient care at the same time.
The BCCGN helps clinicians carry out research studies on unique families and patient populations by providing access to state-of-the-art genomic technologies, assisting with genetic study design and analysis, and offering advice about patient consent and ethics. Partnering with BC Clinical Genomics Network, physicians in BC are beginning to apply genomic technology to address important clinical problems.
Recently, Dr Margot Van Allen at the BC Children’s Hospital and BC Women’s Hospital and Health Centre (C&W) did exactly that when she saw a patient in need of this new technology.
Case data
“John” was the product of a normal pregnancy and birth, but as he got older it became apparent that he had severe mental impairment. He was unable to speak and had seizures, short stature, a thin habitus, and a distinctive phenotype. A variety of tests, including cytogenetic analysis, biochemical studies, blood amino acids, lactate, and ammonia, were undertaken and all results were normal.
An MRI showed John had pachygyria, a nondiagnostic abnormality in brain formation. However, there was one big clue, and that came from the family history. John’s pedigree (Figure 1) demonstrated a classic X-linked recessive pattern of inheritance in which affected males are related to each other through unaffected carrier females. This indicated to Dr Van Allen that John’s condition was most likely the result of a gene carried on the X chromosome.
To investigate further, Dr Van Allen collaborated with the BC Clinical Genomics Network and Dr Neal Boerkoel, a clinician-scientist at C&W. They chose to use a high-throughput SNP (single nucleotide polymorphism) genotyping technology, an extremely robust and relatively inexpensive way to find out where this particular gene is on the X chromosome using linkage analysis.
Genes and single nucleotide polymorphisms
Our genetic material (or genome) is packaged into 23 pairs of chromosomes, one inherited from each parent. Each of these chromosomes consists of a long double-stranded DNA chain twisted into the shape of a double helix (Figure 2). Each DNA molecule contains thousands of genes. DNA itself is made up of a sequence of nucleotide bases—adenine (A), thymine (T), cytosine (C), and guanine (G)—attached by deoxyribose-phosphate linkages.
The sequence of bases on one strand matches base for base with a complementary sequence on the other strand, with A always pairing with T, and C always pairing with G.
The DNA sequence in each of us is 99.5% identical to that of another person. Of the remaining 0.5%, one of the most common variations involves single base changes called single nucleotide polymorphisms (Figure 3). SNPs occur once in about every 1000 bases on average and each of us has about 6 million differences like this in our genome.
The vast majority of these changes are normal variations that do not cause disease. These SNPs are very stable and can be passed on from one generation to the next. Thus, they can be used as markers in SNP genotyping tests.
SNP genotyping platform
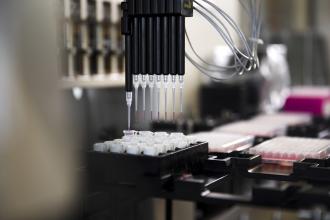
SNP genotyping can be used to look for common variations that may be located very close to a mutant gene that is causing disease in a patient. Numerous methods are currently in use for SNP genotyping.[1] One of these methods,[2] a high-throughput SNP genotyping assay, involves cutting an individual’s DNA into small fragments and labeling them with fluorescent molecules that permit the four bases to be distinguished (Figure 4).
The labeled fragments recognize specific SNPs by “hybridizing” (combining) to each “bead” (a spot on a microchip), which has been precoated with specific reference DNA whose location is known on the genome. The individual’s labeled DNA fragments find their complementary match on the beads, resulting in the generation of a fluorescent signal.
Hundreds of thousands of these beads are tested at once on specially designed microchips. Computer analysis of the fluorescent signals determines an individual’s SNP genotype at each of those thousands of different locations across the entire genome.
This technology can be applied to a variety of different studies, including linkage analysis,[3] which identifies SNPs that are linked to a gene of interest. If several members in a family are affected by a particular disease, then the same SNP will follow the disease gene as it is passed from one family member to another. Knowing which SNP is linked to the gene and where that SNP is located in the genome determines the location of the disease gene.
Association studies[4] can also be done either in large groups of unrelated patients and controls or within a set of families. In these studies, SNP genotyping can be used to look for SNPs that associate with particular diseases such as heart disease, Alzheimer disease, or diabetes.
Discussion
Using one of the high-throughput SNP platforms, results were obtained for John and his family (Figure 5). The A and G bases listed under each family member are the genotypes from SNPs on the X chromosome. Males have one X chromosome and females have two X chromosomes so there is one set of SNPs for each male and two for each female.
It is clear that there is a region of the genome (the AGAG sequence highlighted in ) that segregates with every affected person and carrier. This linkage study allowed Dr Boerkoel to narrow the area of the X chromosome that is involved to a region of approximately 5 million base pairs right at the tip of the X chromosome (Figure 6).
While this is a fairly small area on the X chromosome, which contains almost 155 million base pairs altogether, this segment still contains 240 genes. The task was then to identify the mutation in one of these genes that must be the cause of this disease. Dr Boerkoel continued the investigation in this family by sequencing all of the 240 candidate genes simultaneously using a newly developed high-throughput DNA sequencing platform at the BC Genome Sciences Centre.
The altered gene and specific mutation underlying John’s disease was identified, and finally the “cause” of his condition could be revealed to the family. To do these studies, enormous effort and enthusiasm was needed from many members of the affected family.
The knowledge gathered from the study described here has helped researchers understand how a specific genetic defect may cause the problems in this family and lead to an understanding of the physiology that will, we hope, lead to improved treatment in the near future. It has also allowed clinicians to provide genetic counseling to the family.
Women who are carriers can now get tested to see if they are at risk of having an affected male, and pursue prenatal diagnosis should they wish.
Summary
A research study of a patient and his family conducted at BC Children’s Hospital and BC Women’s Hospital and Health Centre in collaboration with the BC Clinical Genomics Network illustrates how genomic technology can be used and how the results can benefit both families and researchers.
Clinicians involved in studies that identify SNPs associated with a particular disease or risk can help achieve a greater understanding of the condition and, ultimately, help find better therapies for their patients. Families or groups of patients who might be interested in such studies are encouraged to contact the BC Clinical Genomics Network (www.bccgn.ca).
Competing interests
None declared.
References
1. Kim S, Misra A. SNP genotyping: Technologies and biomedical applications. Annu Review Biomed Eng 2007;9:289-320.
2. Shen R, Fan JB, Campbell D, et al. High-throughput SNP genotyping on universal bead arrays. Mutat Res 2005;573:70-82.
3. Nowotny P, Kwon JM, Goate AM. SNP Analysis to dissect human traits. Curr Opin Neurobiol 2001;5:637-641.
4. Wellcome Trust Case Control Consortium, Genome-wide association study of 14,000 cases of seven common diseases and 3,000 shared controls. Nature 2007;447:661-678.
Dr Thomas is the research program manager in the UBC Department of Medical Genetics located at BC Children’s Hospital and BC Women’s Hospital and Health Centre (C&W) in Vancouver. Ms Adam is a genetic counselor and the coordinator for the BC Clinical Genomics Network located at C&W. Ms du Souich is a genetic counselor and clinical assistant professor in the UBC Department of Medical Genetics at C&W. Dr Van Allen is a medical geneticist and professor in the UBC Department of Medical Genetics at C&W. Dr Boerkoel is an associate professor in the UBC Department of Medical Genetics, C&W, and a clinical investigator with the Child & Family Research Institute in Vancouver.