Review Articles
Reimagining congenital cytomegalovirus care in British Columbia
ABSTRACT: Cytomegalovirus is the most common congenital infection in British Columbia and Canada, but current models of care are suboptimal for affected children and families. This review aimed to understand caregiver and health care provider perceptions about current care models for congenital cytomegalovirus. Caregivers (n = 18) and health care providers (n = 26) of children affected by congenital cytomegalovirus were surveyed to explore their perceptions about the current quality of care and any unmet needs and to obtain recommendations for improving care as part of a health system redesign project. Caregivers stressed the need for improved cytomegalovirus education, prevention, and diagnostic processes. Health care providers expressed concerns about testing delays; access to care; and uncertainty regarding diagnosis, clinical practice guidelines, and management of the infection. This review informed the development of a multidisciplinary program at BC Women’s Hospital and Health Centre and BC Children’s Hospital, one of the first in Canada aimed at improving care for families affected by congenital cytomegalovirus.
The current model of care for congenital cytomegalovirus lacks a coordinated approach among teams with specific knowledge about the infection.
Cytomegalovirus is a DNA herpes virus and is endemic worldwide.[1] The virus is typically spread by person-to-person transmission through urine, saliva, genital secretions, or other body fluids.[2] In otherwise healthy children and adults, including pregnant women, primary cytomegalovirus infection is often asymptomatic or may cause minor symptoms such as fever, sore throat, and myalgias. Infants who are affected by congenital cytomegalovirus, where the infection is transmitted perinatally, are at risk of serious morbidity and require timely diagnosis and treatment and long-term follow-up with multidisciplinary teams.[2]
Cytomegalovirus is the most common congenital infection in British Columbia and Canada, affecting approximately 1 in 150 to 240 live births.[2-4] Infants with congenital cytomegalovirus face varying levels of morbidity, ranging from asymptomatic to severe disease. Notably, congenital cytomegalovirus is the leading cause of non-hereditary sensorineural hearing loss, among other significant sequelae that may not be present at birth [Box 1].[2-4]
The seroprevalence of cytomegalovirus among childbearing-age individuals in Canada is estimated to be 40% to 54%, increasing with age and parity. This population faces the risk of virus reactivation or reinfection, leading to intrauterine transmission in 0.5% to 1.5% of pregnancies. Primary infections, affecting approximately 2% of pregnancies, pose a higher risk of transmission, at rates of 30% to 40%, depending on gestational age at time of infection.[2] While routine screening for cytomegalovirus during pregnancy is not standard, up to 74% of pregnant individuals express interest in screening once they are informed of its implications for pregnancy and child development.[5] Despite this, current guidelines from the Society of Obstetricians and Gynaecologists of Canada emphasize the complexity of antenatal cytomegalovirus diagnosis through noninvasive routine screening alongside sonography and amniocentesis.[2]
During pregnancy, congenital cytomegalovirus may be suspected if there is maternal seroconversion; maternal clinical signs; or features suggestive on fetal ultrasonography, including intrauterine growth restriction, echogenic fetal bowel, or brain calcifications. Seroconversion involves detecting the emergence of anti-cytomegalovirus IgG antibodies in individuals who previously lacked them, which indicates recent cytomegalovirus infection.[6] Due to the lack of routine screening for cytomegalovirus in women before conception, documenting cytomegalovirus seroconversion is rare, making primary infection diagnosis challenging.[7] Other tests, including Ig avidity, in which low-avidity IgG antibodies generated at the time of initial infection develop increased avidity with subsequent maturation, and cytomegalovirus IgM antibodies and cytomegalovirus shedding have been studied, but these tests are not standardized, and sensitivity, specificity, and predictive values differ based on prevalence in a population and stage of illness.[7] Additionally, the presence of cytomegalovirus-specific IgM may not indicate primary infection because it can also occur during reactivation or reinfection.[7] Consequently, clinical guidelines do not universally recommend serological screening during pregnancy. Addressing this gap in cytomegalovirus care necessitates further research to establish such guidelines for clinical practice.[8]
Given the challenges with antenatal diagnoses and current evidence that suggests that antiviral treatment has a limited role in antenatally diagnosed cytomegalovirus, the Society of Obstetricians and Gynaecologists of Canada stresses the importance of having multidisciplinary support from experts in maternal-fetal medicine and reproductive infectious diseases and emphasizes the need for increased awareness and education, which are crucial for implementing effective prevention strategies. Previous studies have indicated that informed pregnant individuals show strong willingness to adhere to these strategies.[2]
Following delivery, congenital cytomegalovirus may be clinically suspected in infants with microcephaly, intrauterine growth restriction, hepatosplenomegaly, petechiae, jaundice, hypotonia, and seizures.[1,4] Other clinical signs include abnormal findings on brain imaging, failed newborn hearing screen, chorioretinitis, and, less frequently, optic atrophy or central vision loss.[1,2,4] Laboratory findings often include elevated liver enzymes, thrombocytopenia, and elevated serum bilirubin. Confirmation of congenital cytomegalovirus involves detecting the virus in samples from newborns within the first 3 weeks of life by urine cytomegalovirus polymerase chain reaction (PCR) testing, which is the current gold standard testing modality; alternatives include saliva cytomegalovirus PCR. If not collected within this time frame, cytomegalovirus PCR can be requested from the dried blood spot (DBS) card collected for newborn screen at the time of birth, although it has variable sensitivity and is typically helpful only to rule in congenital cytomegalovirus (a negative test does not rule out congenital cytomegalovirus) given poor test sensitivity.[1,2,4]
Approximately 90% of congenital cytomegalovirus–infected infants are asymptomatic at birth, which makes them challenging to identify initially.[9] However, 10% to 15% of asymptomatic infants may later develop long-term neurological issues, notably hearing loss and developmental delays, which are difficult to assess before the age of 2 years. The remaining 10% of infants with congenital cytomegalovirus are symptomatic at birth, and 36% to 90% of them develop permanent sequelae, such as hearing loss (35%), neurodevelopmental deficits (43%), and vision impairment (6%).[1,2,4]
Early identification of congenital cytomegalovirus is crucial for initiating timely treatment, which has shown significant benefits in improving hearing and neurodevelopmental outcomes when started in the first month of life.[4,10] Infants who are suspected of having congenital cytomegalovirus should undergo diagnostic testing with further evaluation for disease severity, including screening for blood counts and liver enzymes, head imaging, hearing assessment, and ophthalmologic evaluation for potential complications. If seizures or sepsis is suspected, lumbar puncture for central nervous system evaluation is recommended.[4]
Expert opinions vary on indications for initiation of congenital cytomegalovirus treatment. Mildly symptomatic cases, involving one or two systems with transient and mild features, typically do not require treatment. However, moderately to severely symptomatic cases, characterized by central nervous system involvement, chorioretinitis, or multisystem disease, usually warrant treatment. The initiation of treatment for hearing loss alone remains debated. According to Canadian Paediatric Society guidelines, treatment with ganciclovir or valganciclovir for a total of 6 months is recommended for eligible cases.[4,10]
Infants with moderate to severe congenital cytomegalovirus should have timely referral to a multidisciplinary team comprising pediatricians; infectious diseases specialists; audiologists; ear, nose, and throat specialists; and infant development programs. Infants who do not meet treatment criteria because they are mildly symptomatic or asymptomatic are still at risk for adverse outcomes and need ongoing hearing and developmental surveillance, as well as general pediatric care. This approach enables early detection of late-onset or progressive sequelae and facilitates prompt intervention and rehabilitation to improve medical, developmental, and educational outcomes.[1,9,11] However, identifying asymptomatic or mildly symptomatic infants with congenital cytomegalovirus can be challenging. Two provinces have implemented routine DBS-based screening for all infants: Ontario, since 2019, and Saskatchewan, since 2022. While many centres perform targeted screening for infants who fail the newborn hearing screen, this strategy misses more than half of those with congenital cytomegalovirus-related sequelae, including hearing loss, who would have benefited from early intervention services.[2]
Research on the lived experience of those affected by congenital cytomegalovirus is limited, but studies have highlighted parental concerns regarding limited cytomegalovirus awareness prior to and during their pregnancies and poor access to cytomegalovirus-knowledgeable health care teams.[12-14] Though anecdotal, rich qualitative reports available through public domains highlight these same concerns, as well as concerns about delays in care and testing and challenges navigating specialist appointments.[15,16] Research has indicated that there is limited knowledge of congenital cytomegalovirus among both the general population and perinatal health care providers, and reports from health care providers cite insufficient expertise as the main reason for avoiding discussions about congenital cytomegalovirus.[2,13,14] However, there is a gap in the literature regarding the perceptions and experiences of caregivers and health care providers who are involved in congenital cytomegalovirus care in Canada.[15,16]
Until 2022, reproductive infectious diseases specialists at BC Women’s Hospital and Health Centre cared for women with possible cytomegalovirus during pregnancy in a BC Women’s physician-only clinic. Infants diagnosed with congenital cytomegalovirus received general pediatric care in the community with consultation from pediatric infectious diseases specialists (and other specialists where needed) at BC Children’s Hospital. Despite being situated on the same campus, these services operated independently. In 2022, with Health System Redesign funding, care of pregnant people with possible cytomegalovirus during pregnancy and outpatient care of infants with congenital cytomegalovirus were combined in a multidisciplinary clinic that had previously developed a women- and family-centred model of care for HIV in a collaborative, cross-campus, multidisciplinary clinic aimed at providing integrated maternal and infant care for perinatal infections.[17] The redesign was informed by focus groups and individual interviews with physicians who care for patients impacted by congenital cytomegalovirus and was supplemented by surveys on the experiences of caregivers and health care providers who care for children with congenital cytomegalovirus in BC and Canada. The inclusion of the perspectives of those with current lived experience within our systems allowed us to examine the strengths and weaknesses of current care models, barriers to access and quality of care, unmet needs, and recommendations for improvement. The findings, in addition to literature reviews, informed the development of a collaborative and multidisciplinary congenital cytomegalovirus care program in BC.
Methods
Data collection
Two online surveys were developed: one for caregivers with lived experience of congenital cytomegalovirus, the other for health care providers who deliver care to families and children affected by congenital cytomegalovirus. The surveys were developed based on a review of the literature and consultation with health care providers, families, and an evaluation/survey expert. The surveys included both closed and open-text questions to capture the respondents’ lived experiences. The final surveys were pretested with health care providers and families to ensure comprehension and ease of completion. The surveys were administered through REDCap between October 2021 and January 2022.
Surveys for caregivers were distributed by newsletter, website, and social media platforms through the Canadian CMV Foundation, a society with expertise in engaging with families with lived experience of congenital cytomegalovirus, and through pediatric and ear, nose, and throat clinics across Canada that care for children affected by congenital cytomegalovirus, as identified through physician networking. Surveys for health care providers were delivered through the BC Pediatric Society and Doctors of BC and through snowball sampling, in which health care providers in the community were identified and asked to recruit others who may have cared for children affected by congenital cytomegalovirus. This project was reviewed by the University of British Columbia Research Ethics Board and was determined to be in keeping with quality improvement work; thus, it did not require a Research Ethics Board review.
Analysis
Data were analyzed descriptively using SPSS Statistics version 25.0. Inferential statistics were not calculated due to small sample sizes, especially when data were cross-tabulated by role, years of experience, and region. Qualitative data from open-text questions were analyzed thematically using inductive techniques. Data were further coded by two independent reviewers (N.B. and S.Z.), and their frequency counts were reported. Any discrepancies in coding were discussed to reach consensus. Codes were further collapsed to develop overarching themes and subthemes.
Results
Caregiver perspectives
In total, 25 surveys were collected from caregivers. Seven participants were excluded because they did not complete the survey or they were living outside of Canada. The remaining 18 participants either were from Ontario (n = 8), Alberta (n = 3), Quebec (n = 1), or Yukon (n = 1) or did not disclose their location (n = 5). Due to the sampling method, the response rate could not be calculated. Eleven participants lived in urban locations; two lived in rural communities. All participants had some level of postsecondary education, ranging from technical education to university graduate degrees.
Sixty-one percent of caregivers had a child diagnosed with congenital cytomegalovirus within the first month of life; 39% had a later diagnosis. Before pregnancy, 89% of participants (n = 16) had limited knowledge of cytomegalovirus, and only 11% (n = 2) recalled receiving cytomegalovirus education from their health care provider during pregnancy. After diagnosis, survey respondents saw multiple subspecialists, including family physicians; ear, nose, and throat specialists; general pediatricians; pediatric infectious diseases specialists; neonatologists; neurologists; ophthalmologists; psychologists; and audiologists, but 28% (n = 5) felt their providers were unable to adequately address their questions about congenital cytomegalovirus. Respondents also found it challenging to arrange follow-up tests and appointments with their many health care professionals. Improving education and awareness of cytomegalovirus infection during pregnancy was identified as the most crucial need for improving care; it was recommended by 89% (n = 16) of participants. These themes were consistently highlighted in the qualitative survey responses:
- “No health professional ever mentioned [cytomegalovirus] during pregnancy. I had not heard of the virus until my son’s sudden hearing loss at 3 months old.”
- “Pregnant people should be advised of [cytomegalovirus], even something as basic as ‘This is what the virus is, this is what it could do to your child in a congenital infection, here are a couple ways of preventing infection (e.g., hand hygiene).’”
Caregivers also found it difficult to navigate supports within their community and desired a more coordinated approach to access their appointments. Respondents experienced stigma and financial burden and felt overwhelmed by the multiple appointments and treatments involved in their child’s care:
- “I also found it difficult to navigate the various supports in my community.”
- “I only wish my nurse in the NICU wasn’t so judgmental with me. That’s the only negative experience I had.”
Health care provider perspectives
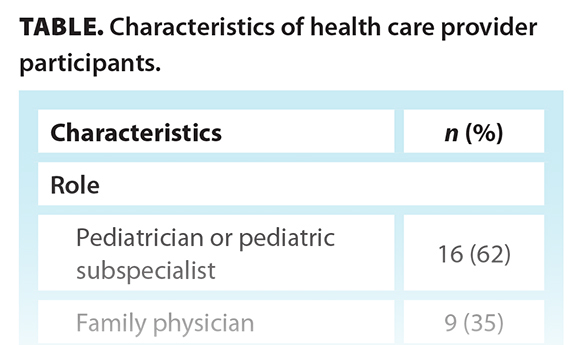 In total, 38 physicians participated in the survey; however, 12 were excluded because they did not complete it [Table]. Although 73% (n = 19) of participants felt confident identifying signs and symptoms of congenital cytomegalovirus, this varied with years of experience: 93% (n = 11) of physicians with 21 years of practice or more were confident identifying signs and symptoms of congenital cytomegalovirus, compared with only 33% (n = 2) who had 5 years of experience or less. Only 54% (n = 14) of all respondents felt confident in knowing which diagnostic tests to order for congenital cytomegalovirus, and 58% (n = 15) felt uncomfortable identifying which children would require treatment. Only 51% (n = 13) and 62% (n = 16) of respondents felt at least somewhat confident in providing short- and long-term outcome counseling, respectively, for children with congenital cytomegalovirus.
In total, 38 physicians participated in the survey; however, 12 were excluded because they did not complete it [Table]. Although 73% (n = 19) of participants felt confident identifying signs and symptoms of congenital cytomegalovirus, this varied with years of experience: 93% (n = 11) of physicians with 21 years of practice or more were confident identifying signs and symptoms of congenital cytomegalovirus, compared with only 33% (n = 2) who had 5 years of experience or less. Only 54% (n = 14) of all respondents felt confident in knowing which diagnostic tests to order for congenital cytomegalovirus, and 58% (n = 15) felt uncomfortable identifying which children would require treatment. Only 51% (n = 13) and 62% (n = 16) of respondents felt at least somewhat confident in providing short- and long-term outcome counseling, respectively, for children with congenital cytomegalovirus.
When asked about system improvement strategies, respondents who had cared for children with congenital cytomegalovirus (n = 11) identified a need for improvements in access to testing, family-focused education resources, and early childhood developmental services. Access to subspecialty advice and timeliness of patient referrals were identified as working well.
Through the open-text questions, respondents highlighted a need for improved standards of care, noted difficulty in establishing a diagnosis, and voiced concerns about delays in access to care. They recommended improving prenatal education, creating a more centralized source of information, and developing guidelines and care pathways. They raised questions about the merit of universal screening at birth:
- “[The] current model seems very inadequate, and most cases are missed.”
- “I believe there are features [of cytomegalovirus] that are easily missed or attributed to other causes.”
Across all BC health regions, concerns were raised about delays accessing care. Some respondents suggested the delays were related to their own lack of understanding about the need for timely diagnosis and access to treatment and to delays in initial hearing assessments and accessing testing results. Furthermore, the need for more education within the physician community was emphasized, including the need for more information on the short- and long-term outcomes of congenital cytomegalovirus and the safety and efficacy of treatment.
Discussion
Health care providers emphasized the need for an improved standard of care for congenital cytomegalovirus, including better prenatal education; centralized sources of information; and accessible, up-to-date guidelines and care pathways. They also identified the need for education to provide better care and counseling to affected families. Many of the needs identified by health care providers were echoed by caregivers, including the need for improved prenatal education, informed counseling, and standardized testing. Both groups expressed concerns about delays in receiving care and challenges in coordinating services.
Updated clinical practice guidelines for congenital cytomegalovirus for health care providers of pregnant individuals and children were published by the Society of Obstetricians and Gynaecologists of Canada in 2021 and the Canadian Paediatric Society in 2020, respectively.[2,4] Additionally, BC-specific resources are available online through the Shared Health Organizations Portal, including information and policy statements on indications for congenital cytomegalovirus testing and workup, guided scripts to support early discussions with families at risk, patient information handouts, logistics and techniques regarding saliva or urine collection for diagnostic assessment, and algorithms to outline follow-up investigations and referrals for infants who test positive.
Efforts to streamline follow-up investigations and referrals for infants who test positive for congenital cytomegalovirus are essential. Surveyed caregivers and health care providers stressed the need for standardized testing and prompt access to care. Currently, only Ontario and Saskatchewan have implemented routine newborn screening for congenital cytomegalovirus. BC and Manitoba have targeted screening programs, but initially asymptomatic infants remain unidentified.[18] Other provinces and territories lack province- and territory-wide screening measures. Debate on the cost-effectiveness of universal screening persists, despite higher disease burden of many screened disorders.[11] Research on the economic impact of congenital cytomegalovirus in Canada is limited, but international studies suggest that universal screening can lead to substantial cost savings by reducing unnecessary tests and supporting children at risk of late-onset hearing loss with appropriate medical, therapeutic, and educational interventions.[11,19]
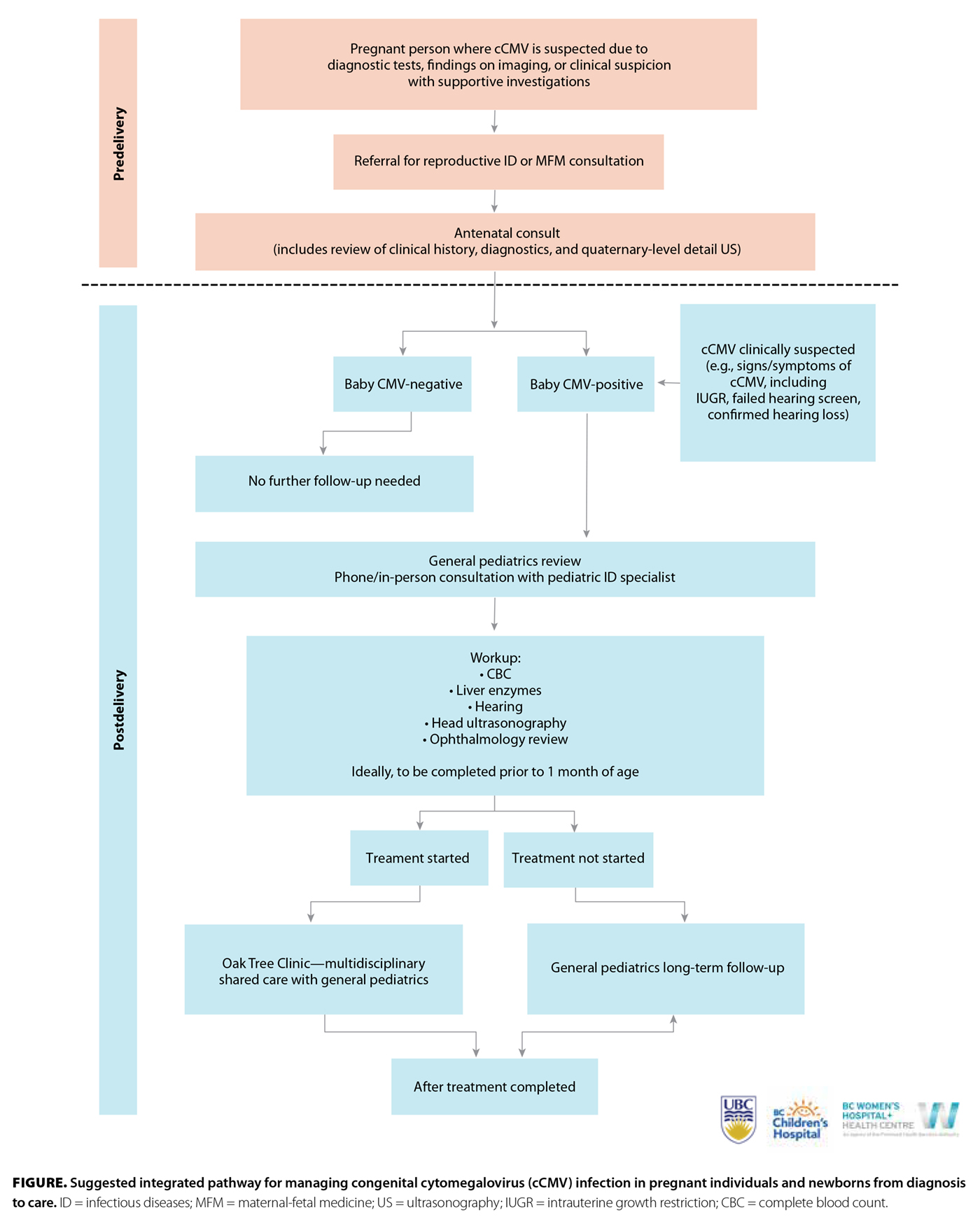 BC Women’s and BC Children’s implemented a cross-campus multidisciplinary service aimed at providing integrated maternal and infant care for congenital cytomegalovirus and other perinatal infections through the Oak Tree Clinic [Box 2; Figure]. The clinic provides shared care in collaboration with community obstetricians, family physicians, midwives, and maternal-fetal medicine specialists across the province, and pediatricians, otolaryngologists, the BC Early Hearing Program, and other pediatric subspecialists. It aims to expand the care provided for reproductive or congenital infectious diseases, including cytomegalovirus, with the aim of facilitating access to comprehensive congenital cytomegalovirus care, including in-person and telephone consultations for pregnant people, caregivers, and children. The clinic includes nursing, pharmacy, dietitian, and social work support. Access to up-to-date and easily understandable resources that are tailored to caregivers and families at key stages of their cytomegalovirus journey are also provided [Box 2; Figure].
BC Women’s and BC Children’s implemented a cross-campus multidisciplinary service aimed at providing integrated maternal and infant care for congenital cytomegalovirus and other perinatal infections through the Oak Tree Clinic [Box 2; Figure]. The clinic provides shared care in collaboration with community obstetricians, family physicians, midwives, and maternal-fetal medicine specialists across the province, and pediatricians, otolaryngologists, the BC Early Hearing Program, and other pediatric subspecialists. It aims to expand the care provided for reproductive or congenital infectious diseases, including cytomegalovirus, with the aim of facilitating access to comprehensive congenital cytomegalovirus care, including in-person and telephone consultations for pregnant people, caregivers, and children. The clinic includes nursing, pharmacy, dietitian, and social work support. Access to up-to-date and easily understandable resources that are tailored to caregivers and families at key stages of their cytomegalovirus journey are also provided [Box 2; Figure].
Study limitations
Our surveys, while informative for program design, had limitations. Sampling through advocacy organizations may introduce selection bias and potentially skew results toward highly educated individuals. A lack of BC participants was mitigated by including national respondents, although we expect that caregivers’ wishes and recommendations for improving care would likely be similar across the country. Additionally, the survey method may have hindered participation by those with limited time and resources, including electronic access to the survey. Although the response rate could not be computed due to the sampling method used, the overall number of survey responses was lower than expected. Furthermore, caregivers represented mainly urban populations, which limited comparisons with rural communities, although health care providers highlighted rural-specific challenges in accessing care and multidisciplinary support. It is critical that interventions for congenital cytomegalovirus care address rural barriers.
Conclusions
Despite our study’s limited sample size, the qualitative data provided valuable insight into caregiver and health care provider perspectives on care for congenital cytomegalovirus, which align with concerns raised by those in previous studies outside of BC and Canada. The current model of care across BC and Canada is lacking a coordinated approach among teams with specific knowledge about cytomegalovirus. In this study, both health care providers and patient caregivers advocated for improved models of care that include better education, both antenatally and perinatally; increased health care provider awareness of congenital cytomegalovirus; better standards of testing; and greater coordination of care among health care services. These findings guided the design of combined maternal and infant care for congenital cytomegalovirus in BC through the Oak Tree Clinic as we work toward improved standards of care for congenital cytomegalovirus in BC and across Canada.
Competing interests
None declared.
BOX 1. Important sequelae impacting children affected by congenital cytomegalovirus.
- Sensorineural hearing loss
- Epilepsy
- Cerebral palsy
- Neurodevelopmental disabilities
- Intellectual delay
- Developmental delay
- Visual impairment
BOX 2. Resources and roles provided by the multidisciplinary teams involved in the care pathway for congenital cytomegalovirus at the Oak Tree Clinic.
- The Oak Tree Clinic at BC Women’s Hospital and Health Centre provides specialized clinical care to women who may have cytomegalovirus in pregnancy and infants with a new congenital cytomegalovirus diagnosis. For further information and referrals, see www.bcwomens.ca/our-services/specialized-services/oak-tree-clinic.
- BC Women’s reproductive infectious diseases specialists can provide consultations for people who may have cytomegalovirus or other infections during pregnancy.
- BC Children’s Hospital’s pediatric infectious diseases specialists can provide phone or in-person consultations for inpatients with congenital cytomegalovirus.
This article has been peer reviewed.
 |
| This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. |
References
1. Davis NL, King CC, Kourtis AP. Cytomegalovirus infection in pregnancy. Birth Defects Res 2017;109:336-346.
2. Boucoiran I, Yudin M, Poliquin V, et al. Guideline No. 420: Cytomegalovirus infection in pregnancy. J Obstet Gynaecol Can 2021;43:893-908.
3. Sorichetti B, Goshen O, Pauwels J, et al. Symptomatic congenital cytomegalovirus infection is underdiagnosed in British Columbia. J Pediatr 2016;169:316-317.
4. Barton M, Forrester AM, McDonald J. Update on congenital cytomegalovirus infection: Prenatal prevention, newborn diagnosis, and management. Paediatr Child Health 2020;25:395-396.
5. Beaudoin ML, Renaud C, Boucher M, et al. Perspectives of women on screening and prevention of CMV in pregnancy. Eur J Obstet Gynecol Reprod Biol 2021;258:409-413.
6. Hyde TB, Schmid DS, Cannon MJ. Cytomegalovirus seroconversion rates and risk factors: Implications for congenital CMV. Rev Med Virol 2010;20:311-326.
7. Munro SC, Hall B, Whybin LR, et al. Diagnosis of and screening for cytomegalovirus infection in pregnant women. J Clin Microbiol 2005;43:4713-4718.
8. Xie M, Tripathi T, Holmes NE, Hui L. Serological screening for cytomegalovirus during pregnancy: A systematic review of clinical practice guidelines and consensus statements. Prenat Diagn 2023;43:959-967.
9. Fowler KB, Boppana SB. Congenital cytomegalovirus infection. Semin Perinatol 2018;42:149-154.
10. Kimberlin DW, Jester PM, Sánchez PJ, et al. Valganciclovir for symptomatic congenital cytomegalovirus disease. N Engl J Med 2015;372:933-943.
11. Cannon MJ. Congenital cytomegalovirus (CMV) epidemiology and awareness. J Clin Virol 2009;46(Suppl 4);S6-S10.
12. Vandrevala T, Barber V, Mbire-Chigumba E, et al. Parenting a child with congenital cytomegalovirus infection: A qualitative study. BMJ Paediatr Open 2020;4:e000844.
13. Wizman S, Lamarre V, Coic L, et al. Awareness of cytomegalovirus and risk factors for susceptibility among pregnant women, in Montreal, Canada. BMC Pregnancy Childbirth 2016;16:54.
14. Pesch MH, Anderson C, Mowers E. Improving obstetric provider congenital cytomegalovirus knowledge and practices. Infect Dis Obstet Gynecol 2020;2020:8875494.
15. CMV Canada. News and stories. Accessed 22 May 2023. https://cmvcanada.com/blog.
16. National CMV Foundation. Blog. Accessed 22 May 2023. www.nationalcmv.org/resources/blog.
17. Kestler M, Murray M, Money D, et al. The Oak Tree Clinic: The envisioned model of care for women living with human immunodeficiency virus in Canada. Womens Health Issues 2018;28:197-198.
18. Vaudry W, Lee BE, Rosychuk RJ. Congenital cytomegalovirus infection in Canada: Active surveillance for cases diagnosed by paediatricians. Paediatr Child Health 2014;19:e1-e5.
19. Gantt S, Dionne F, Kozak FK, et al. Cost-effectiveness of universal and targeted newborn screening for congenital cytomegalovirus infection. JAMA Pediatr 2016;170:1173-1180.
Dr Benson completed this project during her residency in the Department of Pediatrics, Faculty of Medicine, University of British Columbia, BC Children’s Hospital, and is now a pediatrician working in the Department of Pediatrics, BC Women's Hospital and Health Centre. Dr Sauvé is a clinical assistant professor with the Division of Infectious Diseases, Department of Pediatrics, Faculty of Medicine, UBC, BC Children’s Hospital. Dr Elwood is a clinical assistant professor in the Department of Obstetrics and Gynaecology, BC Women’s Hospital and Health Centre, Faculty of Medicine, UBC. Dr Ziabakhsh is an evaluation specialist, population and global health, BC Women’s Hospital and Health Centre.
Corresponding author: Dr Natasha Benson, natasha.benson@alumni.ubc.ca.
