Original Research
Province-wide implementation of the Vancouver Chest Pain Rule
ABSTRACT
Background: The Vancouver Chest Pain Rule is designed to safely reduce hospital admissions of emergency department patients with chest pain. We describe the impact of provincial implementation of the Vancouver Chest Pain Rule on hospital admissions.
Methods: From 2017 to 2018, in 29 British Columbia emergency departments that had a wide range of patients and resources, we encouraged the use of the Vancouver Chest Pain Rule via a coordinated campaign that included in-person meetings, webinars, and online messaging. In a retrospective cohort, we collected all chest pain patients from 2016 to 2017 (before) and 2018 to 2019 (after) for the primary outcome of 30-day hospital admission.
Results: We collected 94 058 (before) and 90 170 (after) visits. Median ages (56), gender (female: 50%), and comorbidities were similar. The admission rate decreased from 23.7% to 22.5% (relative decrease 5.3%; absolute decrease 1.3%).
Conclusions: An organized implementation of the Vancouver Chest Pain Rule was associated with a 5.3% relative reduction in hospitalizations, which translates to 1300 fewer hospitalizations annually.
Provincial implementation of the Vancouver Chest Pain Rule was associated with 1300 fewer hospitalizations annually and fewer consultations, follow-up visits, diagnostics, and adverse cardiac events.
Background
Approximately 5% of North American emergency department visits involve the evaluation of acute chest pain,[1] which translates to 90 000 annual visits for chest pain in British Columbia.[2] While few of these patients will have an acute coronary syndrome, to ensure safety, many will undergo prolonged observation and intensive testing. In low-risk patients, these tests may be unnecessary, lead to false positives, and divert resources from higher-risk patients in the emergency department. Various scoring systems have been devised to identify chest pain patients who are at low risk and can be safely discharged from the emergency department with little follow-up testing.[2-9]
In particular, use of the HEART score, which provides 6-week estimates of acute coronary syndrome risk for chest pain patients, has been popular, and implementation of HEART-based risk scores[8,9] to standardize emergency department management of chest pain patients has resulted in either no change[10] or some decreases in hospital admissions, while maintaining safety.[11-13] While these studies have typically been conducted in a small number of motivated academic sites, it is unclear whether such decreases would be achievable across a wider geographic setting with many emergency departments, many of which have limited resources. However, the HEART score can also be challenging to use in a clinical sense: even the lowest-risk patients have a 1.7% risk of acute coronary syndrome within 6 weeks.[8,9] Should an emergency physician discharge a patient back to primary care under these circumstances, or should the patient be admitted to hospital for additional testing?
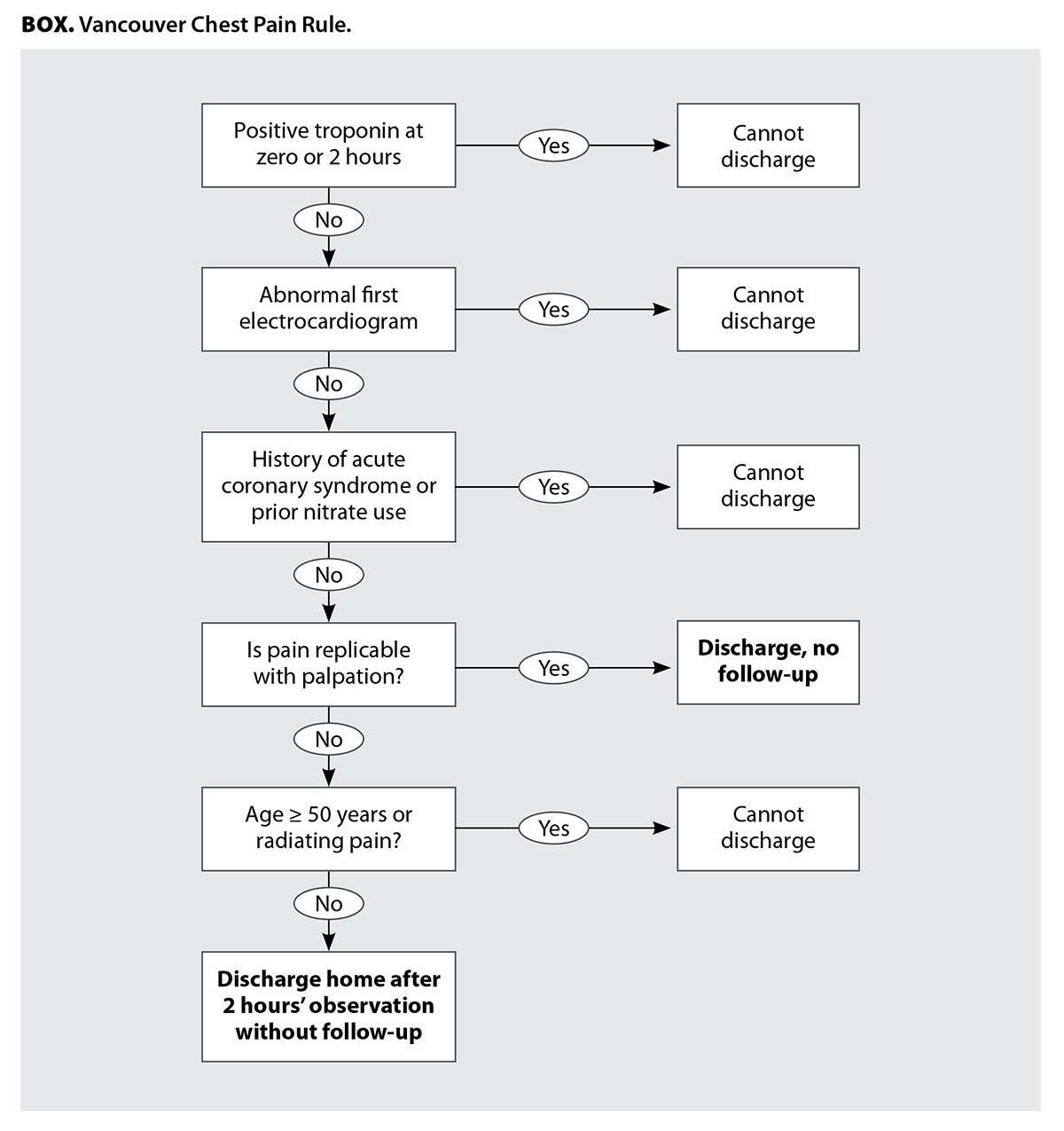 In contrast, the Vancouver Chest Pain Rule [Box], which was derived[7] and validated,[7,14] does not provide acute coronary syndrome risk estimates per se. Rather, it provides physicians with guidance on when to safely discharge patients without additional investigations (such as stress tests) or hospital admission. The main goal of the Vancouver Chest Pain Rule is to reduce admissions of low-risk patients. The rule is more than 99% sensitive and more than 20% specific for acute coronary syndrome.[7,14] We hypothesized that if we conducted an organized campaign to promote use of the Vancouver Chest Pain Rule by BC emergency department physicians and regional leaders, this would be associated with a lower 30-day hospital admission rate and a lower emergency department revisit rate and stress test rate, without a change in mortality. Recently, across 13 Southern California sites, all within the same organization with the same electronic medical record, the introduction of a HEART-based pathway reduced admissions from 14.7% to 13.2%, a relative 10% decrease.[13] Considering our setting was far more diverse in terms of population, geography, distance, resources, and medical informatics, we felt that a 5% relative decrease in hospital admissions was reasonable.
In contrast, the Vancouver Chest Pain Rule [Box], which was derived[7] and validated,[7,14] does not provide acute coronary syndrome risk estimates per se. Rather, it provides physicians with guidance on when to safely discharge patients without additional investigations (such as stress tests) or hospital admission. The main goal of the Vancouver Chest Pain Rule is to reduce admissions of low-risk patients. The rule is more than 99% sensitive and more than 20% specific for acute coronary syndrome.[7,14] We hypothesized that if we conducted an organized campaign to promote use of the Vancouver Chest Pain Rule by BC emergency department physicians and regional leaders, this would be associated with a lower 30-day hospital admission rate and a lower emergency department revisit rate and stress test rate, without a change in mortality. Recently, across 13 Southern California sites, all within the same organization with the same electronic medical record, the introduction of a HEART-based pathway reduced admissions from 14.7% to 13.2%, a relative 10% decrease.[13] Considering our setting was far more diverse in terms of population, geography, distance, resources, and medical informatics, we felt that a 5% relative decrease in hospital admissions was reasonable.
Methods
Setting and study type
To examine potential decreases in hospital admissions for chest pain patients after the dissemination of information on the Vancouver Chest Pain Rule, we completed a retrospective analysis using linked databases in BC, which had a population of approximately 5 million during the study period. BC has more than 100 emergency departments, which are remarkably diverse. Twenty-nine emergency departments—including the five sites that have full cardiovascular capability—report to a provincial database and serve more than 90% of BC’s population. The 12 largest sites are staffed with board-certified emergency physicians and cardiologists; other sites have substantial proportions of primary care physicians that staff emergency departments and may have internists rather than cardiologists. All sites have at least telephone access to an on-call cardiologist, and although patients at such sites can be admitted to an internal medicine ward, those who require coronary interventions must be transported to one of the five sites with full cardiovascular capability.
For patients with potential ischemic chest pain, Canadian emergency physicians employ unstructured judgment and typically have wide latitude in obtaining emergency department–based investigations and treatments, hospital-based consultations, and medication adjustments. Emergency physicians also have an array of options for outpatient follow-up, including cardiology consultations; exercise stress testing, which is widely available; and nuclear medicine scanning, stress echocardiography, and coronary computed tomography angiography, which are available at only a few large centres.
If the emergency physician deems the patient at low risk of acute coronary syndrome, the patient’s consultations and investigations are deferred to the outpatient setting. (Consultations and outpatient tests are typically available within 2 weeks, but patients with worsening symptoms during that period are instructed to return to hospital for additional evaluation and possible admission.) Consequentially, index visit admissions are generally reserved for high-risk patients, such as those with acute myocardial infarctions and unstable angina; in Canada, the admission rate is approximately 25%.[2,15]
Intervention
Emergency Care BC[16] (formerly known as the BC Emergency Medicine Network, which was governed and funded by the BC Academic Health Science Network) is now a Health Improvement Network in the Provincial Health Services Authority with the goal of improving emergency care in BC. It has more than 1000 physician members and, as a learning health system, acts as an information exchange and knowledge implementation platform to promote best practices across the province’s diverse emergency departments. From late 2017 to mid-2018, emergency physician topic experts visited sites, including rural and remote areas; held town hall meetings and webinars; and provided relevant educational information about the Vancouver Chest Pain Rule to emergency department heads and regional leaders. The Emergency Care BC website and social media feeds encouraged the use of the Vancouver Chest Pain Rule. Emergency Care BC leadership sought feedback on the knowledge translation approach and made changes to it as suggested by physicians, emergency department heads, and regional leaders.
Patient selection
Using the validated National Ambulatory Care Reporting System,[17] we collected consecutive patients from 1 September 2016 to 31 August 2019 who presented with Canadian Emergency Department Information System[18] complaints 003 (chest pain with cardiac features) or 004 (chest pain with noncardiac features) or ICD-10A codes R07.4 (chest pain), I21.9 (acute myocardial infarction), I20.0 (unstable angina), or I20.9 (angina pectoris). Patients could be included if they re-presented at least 30 days after the index emergency department visit. We linked these patients to several provincial databases. We used the Canadian Institute for Health Information Discharge Abstract Database[19] to identify all hospital admissions, emergency department visits, and cardiac procedures up to 30 days past the index emergency department visit. We also used this database to identify cardiac procedures in the year prior to the index emergency department visit.
We used the provincial Medical Services Plan billing database[20] to ascertain cardiovascular comorbidities identified over the year prior to the emergency department visit, but we realized this would result in a systemic undercount of all comorbidities, because patients may not have visited their primary care physician, internist, or cardiologist during that time frame. However, the main purpose of this information was not to ascertain the exact risk profile of each patient, but to ensure that the before and after groups were reasonably similar. The same database was also used to obtain information on stress tests and cardiology, internist, and primary care visits in the 30 days after the index emergency department visit. All data were provided as aggregated rather than line items.
Outcomes
The primary outcome was 30-day admissions, defined as the sum of admissions at the index emergency department visit and additional hospital admissions within 30 days. We reasoned this might include patients who were admitted at the index visit and again within 30 days or patients who were readmitted with a noncardiac cause, but we would not expect a difference in this ratio between study periods. While Poldervaart and colleagues[10] documented no before–after changes, Mahler and colleagues[11,12] and Sharp and colleagues[13] estimated at least 10% relative decreases in admissions; however, we expected lower decreases, given that Canadian chest pain admission rates are already far lower at baseline[3,14] than those described by Mahler and colleagues and Sharp and colleagues.[11-13]
We measured additional outcomes at 30 days: emergency department revisits after index visit discharge, the number of stress tests conducted, follow-up visits (cardiology, internal medicine, and primary care), revascularizations (percutaneous coronary intervention and coronary artery bypass grafting), and mortality. We expected the latter two outcomes to have low absolute numbers.
Data analysis
We used Microsoft Excel 2019 (Microsoft Corporation, Redmond, WA) and SAS version 9.4 (SAS Institute Inc., Cary, NC) for data entry and analysis. We reported discrete variables as percentages and continuous variables as means with standard deviations if normally distributed or as medians with interquartile ranges otherwise. The unit of analysis was the patient encounter. We had no way to address missing data. Given that the educational intervention took place from late 2017 to mid-2018, we used a “before” time period of 1 September 2016 to 31 August 2017 and an “after” time period of 1 September 2018 to 31 August 2019. We used appropriate testing, including Student’s t tests, chi-square tests, and Fisher exact tests, to ascertain any differences. Due to the retrospective nature of this study, the wide setting, and the prolonged data collection period, we expected to obtain very large numbers of patients.
The Research Ethics Board of Providence Health Care approved this study.
Results
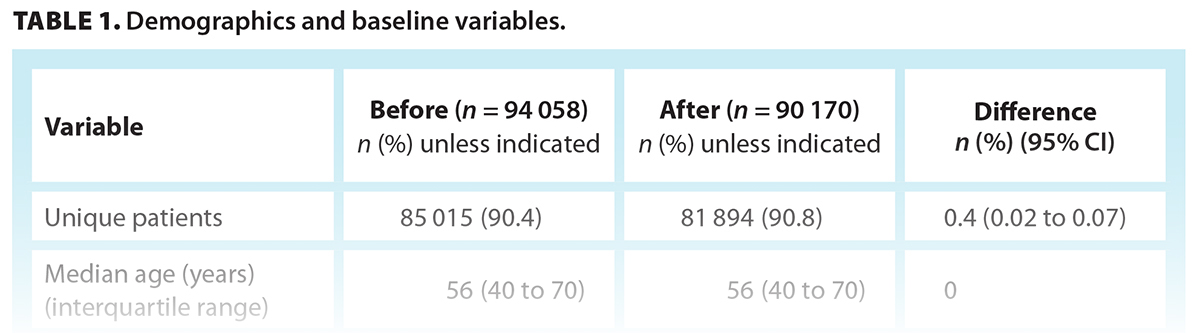
The 2016–2017 (before) cohort had 94 058 encounters (85 015 unique patients); the 2018–2019 (after) cohort had 90 170 encounters (81 894 unique patients). The median age in both cohorts was the same, and the proportion of females was similar [Table 1].
The proportion of patients with same-year diagnoses of high blood pressure and diabetes in each cohort was similar, as was the proportion with same-year percutaneous coronary intervention and coronary artery bypass graft [Table 1].
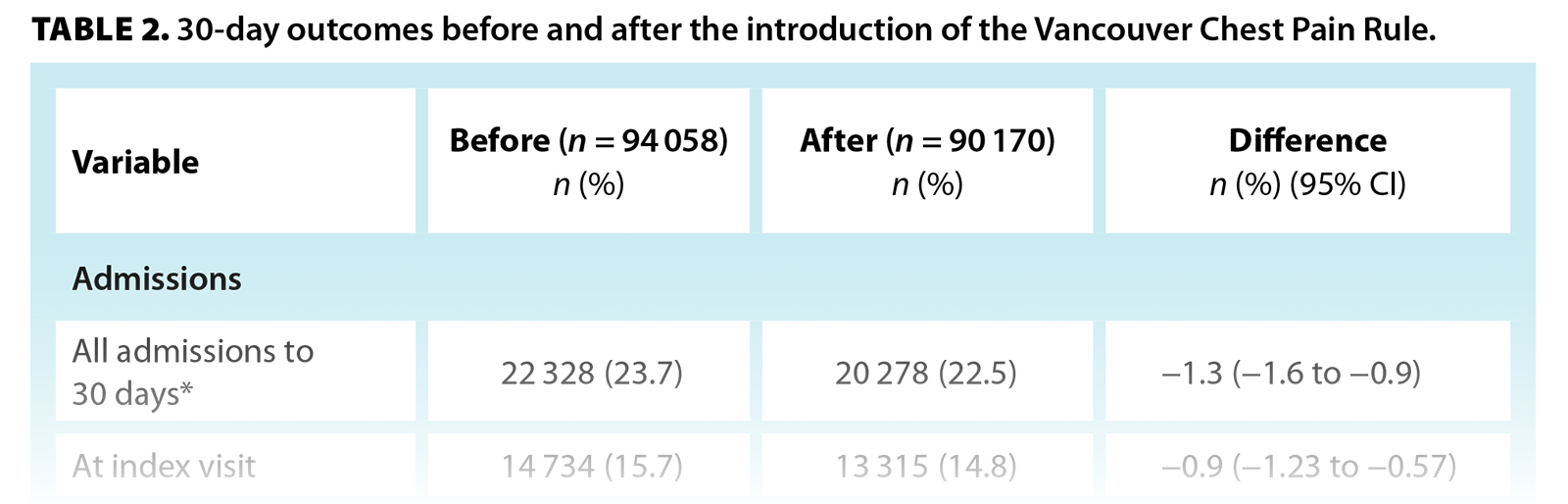
Overall, 23.7% of encounters (95% CI, 23.4 to 24.0) in the before cohort and 22.5% (95% CI, 22.2 to 22.8) in the after cohort were admitted by 30 days, an absolute reduction of 1.3% and a relative reduction of 5.3%. The proportion of patients admitted at the index visit declined from 15.7% to 14.8%, a decrease of 0.9% and a relative reduction of 5.6%; the proportion of patients admitted after the index visit up to 30 days declined from 8.1% to 7.7%, a decrease of 0.4% and a relative reduction of 4.3%. The proportion of patients that revisited an emergency department for any cause within 30 days declined from 30.4% to 29.4%, a decrease of 1.0% and a relative reduction of 3.3%. All declines were statistically significant [Table 2].
At 30 days, 77.9% of follow-up physician visits took place in the before period and 77.2% occurred in the after period, a significant reduction of 0.6%. The proportion of follow-up diagnostics decreased from 28.3% to 26.6%, an absolute reduction of 1.7% and a relative reduction of 6.0% [Table 2].
Overall, in the before and after cohorts, 4.7% and 4.8% of patients, respectively, had percutaneous coronary intervention and 2.2% and 2.0% of patients, respectively, had a coronary artery bypass graft; neither was a significant change. Thirty-day mortality in both groups was 0.6%. Major adverse cardiac events decreased significantly from 3.5% in the before cohort to 3.2% in the after cohort, a reduction of 0.3% (95% CI, −0.47 to −0.14) [Table 2].
Discussion
Our analysis of nearly 185 000 patients in BC who were admitted to the emergency department with potential ischemic chest pain indicated that the use of the Vancouver Chest Pain Rule was associated with a relative 5.3% reduction in 30-day hospital admissions, which translates to approximately 1300 fewer hospitalizations annually. In addition, there were significant decreases in consultations, follow-up visits, diagnostic testing, and major adverse cardiac events. Given that the typical length of stay in a Canadian hospital for a patient admitted with chest pain is 2 to 6 days,[17] in BC, which has a population of 5 million people and more than 90 000 hospital visits for chest pain annually, implementation of the Vancouver Chest Pain Rule would likely save 2600 to 7800 hospital bed days; hundreds of hospital-to-hospital transfers from smaller sites to larger, angiography-capable sites; thousands of follow-up visits and diagnostic investigations; and 900 emergency department return visits per year—along with millions of dollars—while maintaining similar safety outcomes.
Prior work has shown that implementation of an organized approach to emergency department chest pain management has reduced hospitalizations, although these approaches have been used at single sites or in health networks that have large, reasonably comparable emergency departments.[10-13,21] Poldervaart and colleagues used a stepped-wedge design to explore the effect of using a HEART-based clinical pathway in emergency departments in 10 Netherlands sites, ranging from 500 to 1200 inpatient beds, for patients with chest pain.[10] No differences between the before and after cohorts were found, and adjusted admissions decreased by a nonsignificant 0.7%.[10] At a single North Carolina emergency department with more than 100 000 annual visits, Mahler and colleagues randomly assigned 282 chest pain patients to a HEART-based pathway versus usual care and reported a decrease in index admissions from 78% to 60%, a commensurate decrease in objective cardiac testing, and no change in major adverse cardiac events or mortality at 30 days.[11] Finally, Sharp and colleagues studied more than 65 000 chest pain patients across 13 emergency departments in California that implemented the HEART score and reported that the index visit admission rate declined from 14.7% to 13.2%, an absolute decrease of 1.5% and a relative decrease of 10.2%, without an increase in missed myocardial infarctions or mortality.[13]
Non-HEART-based pathways have also been described. Than and colleagues introduced an acute coronary syndrome pathway at seven New Zealand sites, which involved more than 31 000 patients, and reported that the proportion of patients who had a length of stay less than 6 hours increased from 8% to 18%,[21] but the authors did not comment on hospital admissions. In a setting more similar to our study population and using similar methodology, Greenslade and colleagues found that the introduction of high-sensitivity troponins reduced the length of stay across 21 Queensland sites by 1.9 hours; however, since the admission rates decreased from 6.8% to 5.7%, it is reasonable to assume that the patients were systematically healthier than our cohort. Importantly, neither study reported an increase in downstream myocardial infarctions or mortality.[22]
It is critical to note that compared with our province-wide investigation, prior studies (except for the Queensland study[22]) have been conducted in large academic sites—typically with far more on-site cardiovascular resources—and have received more financial, educational, and material support. Our study, which included many smaller sites with few cardiology-specific resources, suggests that interventions to modify clinical pathways and physician behavior may apply across large geographic areas with a wide range of emergency department and hospital types rather than only to strongly motivated academic sites. While our findings require replication in other settings and possibly with other chest pain care pathways, overall, this could preserve scarce resources for higher-risk patients while alleviating unnecessary hospitalization and ancillary testing for lower-risk patients, which may represent a significant opportunity for system-wide capacity improvement.
Study limitations
This study was undertaken in a single Canadian province with universal health care; therefore, the results may not be reproducible elsewhere. Typical limitations of a before–after study design apply, and we cannot conclusively demonstrate that our campaign directly led to a reduction in hospital admissions. Cluster randomization or stepped-wedge implementation[10] would have provided stronger evidence, but this would have been challenging across our diverse sites. The 70 smallest hospitals—all rural and serving less than 10% of the provincial population—do not submit standardized data, so we could not assess them. Importantly, individual emergency departments and hospitals may have instituted their own protocols to reduce chest pain admissions during the study period, and we cannot account for this potential confounder. Our admission rates may be different from those in other jurisdictions,[11-13] but they are generally comparable with Canadian norms.[15] The Vancouver Chest Pain Rule informs physicians about the need for downstream testing, whereas the HEART score provides an acute coronary syndrome risk estimate; therefore, the two systems have different goals. Our goal was to test whether the Vancouver Chest Pain Rule could reduce admissions; had we implemented and tested the HEART score (or a similar tool), our results may have been different.
We had a 1-year run-in period to liaise with the numerous sites. We did not have access to important traditional data, such as prior cardiac illness, family history, smoking background, initial electrocardiogram, and laboratory biomarkers, and our estimates of comorbidities and prior cardiac interventions were obviously low. While we have little reason to suspect that these variables would be substantially different between the two cohorts, the lack of such baseline data precluded any adjusted analysis of baseline risk at an individual level. Furthermore, since we had no line-item data, we could not perform an individual- or site-level analysis. Some of our post-index visit admissions may have been unrelated to cardiac disease, but we also would not expect this to differ between time periods. Outcomes are to 30 days, although this is typical for emergency department–based literature regarding cardiovascular issues. Finally, we cannot comment on patient or provider satisfaction, emergency department or hospital length of stay, or costs.
Conclusions
In BC, the organized implementation of the Vancouver Chest Pain Rule was associated with a 5.3% relative reduction in hospitalizations, which translates to 1300 fewer hospitalizations annually, as well as fewer consultations, follow-up visits, diagnostics, and adverse cardiac events.
Competing interests
None declared.
Acknowledgments
The authors gratefully acknowledge the foundational work to optimize emergency care in BC by all those affiliated with the BC Emergency Medicine Network from 2019 to 2023. In April 2023, the BC Emergency Medicine Network transitioned to become Emergency Care BC, a new Provincial Health Services Authority Health Improvement Network, through which these efforts and the advancement of the broader goal of a learning health system in emergency care will continue.
This article has been peer reviewed.
 |
| This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. |
References
1. US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. National hospital ambulatory medical care survey: 2019 emergency department summary tables. Accessed 14 September 2023. www.cdc.gov/nchs/data/nhamcs/web_tables/2019-nhamcs-ed-web-tables-508.pdf.
2. Canadian Institute for Health Information. NACRS emergency department visits and lengths of stay. 2023. Accessed 14 September 2023. www.cihi.ca/en/nacrs-emergency-department-visits-and-lengths-of-stay.
3. Than M, Cullen L, Aldous S, et al. 2-hour accelerated diagnostic protocol to assess patients with chest pain symptoms using contemporary troponins as the only biomarker: The ADAPT trial. J Am Coll Cardiol 2012;59:2091-2098.
4. Jaffery Z, Hudson MP, Jacobsen G, et al. Modified thrombolysis in myocardial infarction (TIMI) risk score to risk stratify patients in the emergency department with possible acute coronary syndrome. J Thromb Thrombolysis 2007;24:137-144.
5. Than M, Cullen L, Reid CM, et al. A 2-h diagnostic protocol to assess patients with chest pain symptoms in the Asia-Pacific region (ASPECT): A prospective observational validation study. Lancet 2011;377(9771):1077-1084.
6. Mahler SA, Miller CD, Hollander JE, et al. Identifying patients for early discharge: Performance of decision rules among patients with acute chest pain. Int J Cardiol 2013;168:795-802.
7. Scheuermeyer FX, Wong H, Yu E, et al. Development and validation of a prediction rule for early discharge of low-risk emergency department patients with potential ischemic chest pain. CJEM 2014;16:106-119.
8. Six AJ, Backus BE, Kelder JC. Chest pain in the emergency room: Value of the HEART score. Neth Heart J 2008;16:191-196.
9. Backus BE, Six AJ, Kelder JC, et al. Chest pain in the emergency room: A multicenter validation of the HEART score. Crit Pathw Cardiol 2010;9:164-169.
10. Poldervaart JM, Reitsma JB, Backus BE, et al. Effect of using the HEART score in patients with chest pain in the emergency department: A stepped-wedge, cluster randomized trial. Ann Intern Med 2017;166:698-697.
11. Mahler SA, Lenoir KM, Wells BJ, et al. Safely identifying emergency department patients with acute chest pain for early discharge. Circulation 2018;138:2456-2468.
12. Mahler SA, Riley RF, Hiestand BC, et al. The HEART pathway randomized trial: Identifying emergency department patients with acute chest pain for early discharge. Circ Cardiovasc Qual Outcomes 2015;8:195-203.
13. Sharp AL, Baecker AS, Shen E, et al. Effect of a HEART care pathway on chest pain management within an integrated health system. Ann Emerg Med 2019;74:171-180.
14. Cullen L, Greenslade JH, Than M, et al. The new Vancouver Chest Pain Rule using troponin as the only biomarker: An external validation study. Am J Emerg Med 2014;32:129-134.
15. Scheuermeyer FX, Innes G, Grafstein E, et al. Safety and efficiency of a chest pain diagnostic algorithm with selective outpatient stress testing for emergency department patients with potential ischemic chest pain. Ann Emerg Med 2012;59:256-264.e3.
16. Abu-Laban RB, Christenson J, Lindstrom RR, Lang E. Emergency care clinical networks. CJEM 2022;24:574-577.
17. Canadian Institute for Health Information. Emergency and ambulatory care. Accessed 14 September 2023. www.cihi.ca/en/topics/emergency-and-ambulatory-care.
18. Grafstein E, Bullard MJ, Warren D, et al. Revision of the Canadian Emergency Department Information System (CEDIS) presenting complaint list version 1.1. CJEM 2008;10:151-173.
19. Canadian Institute for Health Information. Discharge abstract database (DAD) metadata. Accessed 4 March 2023. www.cihi.ca/en/discharge-abstract-database-metadata-dad.
20. British Columbia Ministry of Health. Medical Services Plan data set. Accessed 4 March 2023. www.popdata.bc.ca/data/health/msp.
21. Than MP, Pickering JW, Dryden JM, et al. ICare-ACS (Improving Care Processes for Patients with Suspected Acute Coronary Syndrome): A study of cross-system implementation of a national clinical pathway. Circulation 2018;137:354-363.
22. Greenslade JH, Parsonage W, Foran L, et al. Widespread introduction of a high-sensitivity troponin assay: Assessing the impact on patients and health services. J Clin Med. 2020;9:1883.
Dr Scheuermeyer is an innovation lead with Emergency Care BC and a clinical associate professor in the Department of Emergency Medicine, St Paul’s Hospital and the University of British Columbia. Mr Duncan is a learning health systems data analyst with Emergency Care BC and an adjunct professor in the Department of Emergency Medicine, Vancouver General Hospital and UBC. Dr Abu-Laban is the scientific director of Emergency Care BC and a professor in the Department of Emergency Medicine, UBC. Dr Besserer is an assistant professor in the Department of Emergency Medicine, UBC, and an affiliate assistant professor, Division of Medical Sciences, University of Northern British Columbia. At the time of the study, Ms Drebit was executive director of the BC Emergency Medicine Network. She is currently executive director, strategic business, performance, and operations, at Coast Mental Health. Dr Christenson is a professor in the Department of Emergency Medicine, St Paul’s Hospital and UBC.