Review Articles
Physiotherapy and knee osteoarthritis
ABSTRACT: Knee osteoarthritis is a prevalent and debilitating condition affecting millions of people worldwide. Physiotherapy is a noninvasive intervention that is effective in managing knee osteoarthritis symptoms by aiming to reduce pain, improve function, and enhance quality of life. The main interventions are exercise therapy, including strength training, aerobic exercise, and neuromuscular training, and patient education about self-management strategies, such as weight loss, activity modification, and pain coping skills. Research on the benefits of biomechanical interventions is limited, but walking aids (e.g., canes, crutches, frames, wheeled walkers) are generally considered to be effective in reducing mechanical loading through the knee, relieving pain, improving balance and function, and enhancing independence and safety; evidence of the benefit of shoe inserts is mixed. There is also a lack of high-quality research on the benefits of adjunct therapies such as heat or ice, low-level laser therapy, therapeutic ultrasonography, manual therapy, and acupuncture, but they may be conditionally recommended based on patient preference if they are used in combination with exercise. Individualized and patient-centred care in physiotherapy for knee osteoarthritis is important, and tailored interventions that take into account patient preferences and goals are needed. A combination of several interventions, depending on patient preference, is recommended for optimal outcomes in managing knee osteoarthritis.
Physiotherapy is a safe and effective nonpharmacological intervention that can be used to manage knee osteoarthritis and improve patients’ quality of life.
Osteoarthritis is often diagnosed clinically; its management is guided by symptoms and physical function.[1] The knee is the most common site of self-reported, physician-diagnosed osteoarthritis in BC.[2] Arthritis of the knee not only affects the specific joint, but can also impact overall health. It limits daily activity, particularly walking; participation in sports; and quality of life.
Although osteoarthritis is traditionally associated with older age, it is increasingly recognized as also impacting younger people. International data from the Global Burden of Disease study show that the prevalence of knee osteoarthritis peaks around 50 years of age.[3] The pain and physical impairments associated with knee osteoarthritis can be particularly problematic for younger people who may need to manage their osteoarthritis alongside family and work commitments. Current evidence shows that education, physical exercise, and weight management constitute the first-line approach for managing knee osteoarthritis in all age groups.[4,5]
Physiotherapy plays an integral role in managing and caring for patients with osteoarthritis.[6] Patients may be referred to physiotherapy by a physician or may be self-referred. The primary goals of physiotherapy for knee osteoarthritis are to manage pain, educate the patient about the nature of osteoarthritis and how it affects their knee, and provide tools to help them enhance their quality of life living with osteoarthritis.
Assessment
In the initial visit to the physiotherapist, a clinical history of the patient’s medical condition is taken, including the onset and duration of their knee pain and any aggravating and alleviating factors. Asking about the patient’s general health is crucial for identifying any comorbidities and helping them manage their knee symptoms appropriately. The patient should also be asked if there are any specific challenges or limitations that affect their quality of life at home or at work, and if there are any activities they have had to stop and would like to return to.
The physical assessment consists of evaluating the range of motion and strength of the patient’s whole lower limb, including the knee; observing their gait for any obvious antalgic patterns or compensatory movements; and testing their ability to perform activities of daily living and functional tasks such as getting on and off a chair and negotiating stairs. In addition, any imaging reports should be reviewed.
Treatment
Core treatments for knee osteoarthritis focus on providing relevant education and support, discussing therapeutic exercise and how weight can affect knee osteoarthritis, and making recommendations, if needed, on where to find appropriate weight management information. In a few cases, adjunct therapies may be beneficial, given patient preference, but only if they are used in combination with education and exercise.[1]
Education and support
Physiotherapists can support family physicians in treating knee osteoarthritis by reinforcing patient education about the disease, which includes explaining what it is and, as important, what it is not. This can help patients better understand the disease process, progression, and risk factors, and it counters misconceptions, especially about radiological findings and activity levels.
Education can include information on disease-modifying factors such as exercise (balanced with appropriate rest); the management of activities of daily living; and the benefits and limitations of nonpharmaceutical pain management options, such as braces, shoe inserts, and manual therapies. Educating patients and teaching them self-management techniques enables them to actively participate in their own care, which can be crucial to ensuring their long-term adherence to treatment programs and sustained positive effects on symptoms, impairments, physical activity levels, and comorbidities.[7] Education interventions can be 20% to 30% more effective than using NSAIDs to treat pain in osteoarthritis.[8]
Physiotherapists can also provide ongoing support with managing flare-ups and disease progression over time, including where to find additional information if needed. How people receive this information may also be important, depending on their age. People aged 20 to 55 years prefer emailed and online information about their knee osteoarthritis.[9] Providing written information sheets and referrals to trustworthy websites (e.g., Arthritis Society Canada, Mary Pack Arthritis Program, Canadian Arthritis Patient Alliance, Arthritis Research Canada) is paramount for this age group.[9] In our experience, older patients prefer in-person discussion and typed booklets.
Exercise therapy
The primary goal of exercise therapy is to provide a tailored program that is focused on strengthening the muscles of the legs and improving joint mobility. In collaboration with the patient, physiotherapists can also explore options for aerobic exercise to help improve overall fitness while protecting the knee joint.
Osteoarthritic knees show evidence of increased pro-inflammatory markers and degradative enzymes, which impair the cartilage matrix. In addition to helping maintain bone density and muscle strength, exercise can combat articular cartilage degradation by reducing the concentration of proteins that are hostile to articular health and can result in increases in anti-inflammatory markers;[10] therefore, it is favored in treating osteoarthritis. A meta-analysis of 60 randomized controlled trials that compared 12 types of exercise interventions with no exercise in adults with knee or hip osteoarthritis showed that exercise provided significant benefits over no exercise.[11]
Physiotherapists prescribe certain types of exercise therapy to achieve specific therapeutic goals. For example, muscle weakness may be an important risk factor for knee osteoarthritis and may impair function and increase disease progression.[12] Therefore, the physiotherapist will prescribe appropriate strengthening exercises as part of the primary treatment approach.
Traditional exercise interventions such as strength, aerobic, and mobility training, and some nontraditional forms such as yoga, tai chi, and aquatic training, have all been shown to improve joint symptoms and mobility.[6,7] This in turn can lead to increased quality of life, psychological health, musculoskeletal strength, and body composition, and improved sleep and reduced fatigue. The benefits of therapeutic exercise appear to be greater when general exercise guidelines for healthy adults are met. For example, the Canadian Society for Exercise Physiology’s 24-hour movement guidelines for adults aged 18–64 recommend 150 minutes per week of moderate to vigorous aerobic physical activity, muscle strengthening activities using major muscle groups at least twice per week, and several hours of light activities, including standing.[13] Using a combination of exercises that increase muscle strength, aerobic capacity, and flexibility may be the most effective approach to managing lower limb osteoarthritis.[11] Numerous international organizations, including the Osteoarthritis Research Society International,[4] Ottawa Panel, American College of Rheumatology,[14] and European Alliance of Associations for Rheumatology,[5] recommend using a combination of strengthening and aerobic exercises and some form of mind–body exercise, such as yoga or tai chi.
Therapeutic exercise is safe for patients with knee osteoarthritis and has shown minimal risk of negative consequences.[9] However, since it is common to initially have an increase in joint pain, physiotherapists educate patients about this possibility and explain that despite any initial discomfort, exercise is beneficial for the long-term management of their osteoarthritis.[4,5,13,14] Regular monitoring, reassurance, and exercise modifications to reflect any changes that arise are essential to helping the patient maintain their exercise regimes and activities.
Physiotherapists play an important role in assessing joint function and level of activity in order to prescribe appropriate exercises following FITT (frequency, intensity, type, and time) principles while considering patient preferences.[15] Patient preference regarding level of supervision and mode of exercise may be key predictors in exercise adherence and degree of outcome improvement.[16]
Strength training: Muscle weakness, particularly of the quadriceps, may be an important risk factor for knee osteoarthritis, especially in women. In one study, the quadriceps muscle was on average 20% weaker (even after controlling for body mass and other covariates) in patients with radiographic signs of osteoarthritis and appeared to predate the onset of the disease in women.[12]
Strength training includes progressive force output of the muscles through various exercises to target specific muscle groups. These exercises may involve the use of weights, body weight, or machines, and the application should include appropriate resistance load, number of repetitions, velocity of movements, and frequency of sessions. The benefits of therapeutic exercise appear to be greater when exercise is adequately dosed.[16]
General exercise guidelines for healthy adults recommend a minimum of two and optimally three sets of 8 to 12 repetitions in three sessions per week.[16,17] Strength gains occur from progressive training, and improvements in symptoms and function are directly related to exercise intensity.[18] There is insufficient evidence that any one type of strength training is superior, so physiotherapists can tailor exercise options individually for patients who prefer to use different equipment and/or locations. Future research may add to the existing high-quality evidence of beneficial exercise by providing more detail on exercise treatment parameters, which will assist in prescribing individualized exercise protocols based on patient preference.[16]
Walking: For individuals who are 50 years of age or older, walking can be associated with less frequent development of knee pain.[19] Therefore, physiotherapists often recommend walking as a simple, low-cost exercise option that can be helpful in managing osteoarthritis of the knee; however, it needs to be of sufficient intensity to produce beneficial change.[20] Aerobic walking significantly reduces disability and pain and is associated with a decreased risk of functional limitation.[20]
Running: Whether to continue running is a common question for some patients with knee osteoarthritis, and the myth that running is bad for osteoarthritic knees is still pervasive in the public forum. A 2022 systematic review concluded that “middle-aged runners did not present greater imaging or clinical signs of osteoarthritis compared with non-runner controls.”[21] While some knee osteoarthritis patients stop running due to pain in their knee(s), not all experience the same amount of discomfort. An eight-year study that followed runners over the age of 50 indicated that for some individuals with knee osteoarthritis, running at a self-selected pace was not associated with any increase in pain, and some runners reported some improvement in their pain; there also was no worsening of “radiographically defined structural progression.”[22] These results suggest that self-selected running is probably influenced by knee symptoms; therefore, running at a lower intensity and for shorter durations does not necessarily need to be discouraged among keen runners.[22] Physiotherapists will discuss the risks versus benefits with patients who wish to continue running and will recommend that they run at their preferred speed and at an intensity and distance that are manageable for their symptoms.
To be clear, this section is not intended to advocate for running as a therapeutic modality. It is simply intended to provide information and reassurance for dedicated runners who wish to continue participating in their preferred sport.
Aquatic exercise: Given patient preference, physiotherapists may also suggest water-based training (including swimming, aquafit classes, and pool running). These activities are recommended by the Osteoarthritis Research Society International, American College of Rheumatology, and European Alliance of Associations for Rheumatology to assist in controlling osteoarthritis symptoms.[4,5,14] A meta-analysis of 20 studies showed that aquatic exercise was beneficial for reducing pain and improving physical function, knee extension muscle strength, and walking ability.[23]
Mind–body exercise: Yoga is very popular, and many options are available in most communities. Although there is less high-quality evidence of the benefits of using tai chi and yoga in treating knee osteoarthritis compared with other exercise modalities, research indicates that these forms of exercise may enhance flexibility, balance, self-efficacy, and muscle strength, thereby leading to improved physical function and reduced pain, depression, and anxiety in patients with chronic osteoarthritis.[4,24] Therefore, they are good options for patient exercise programs.
Supervised exercise programs: For some patients, supervised exercise programs may be preferred. One option is Good Life with osteoArthritis in Denmark (GLA:D), an internationally known physiotherapist-led program that originated in Denmark. Following the original protocol from the Danish studies, GLA:D Canada offers programs that include two or three detailed education and self-management sessions delivered by physiotherapists and other health care professionals. Osteoarthritis patients, who can speak as peers, also provide presentations about their personal experience with the program. The program offers twice-weekly supervised exercise sessions (focusing on strengthening and neuromuscular exercises) over a 6-week period.
A 2019 report from GLA:D Canada suggested that, overall, improvements in pain, quality of life, and physical function for patients in Canada who had knee arthritis reflected the type and magnitude of the findings reported by GLA:D in Denmark. “Based on program implementation by clinical sites and participant outcomes to date, the GLA:D program is successfully supporting people with knee osteoarthritis to manage their symptoms, improve their function and enhance their quality of life.”[25] Participants reported a decrease in pain, use of pain medications, use of intra-articular injections, and fear of damaging their knee, and an increase in function and self-efficacy scores.[25]
While these programs can be extremely beneficial for the participants, not everyone will have access to or prefer a supervised exercise program. The Better Management of Patients with Osteoarthritis register shows that home exercise and supervised exercise lead to similar reductions in pain intensity and are more effective than education alone.[26]
Barriers to exercising are common due to patient beliefs, fear of movement, affordability, time commitment, and equality of access. Therefore, physiotherapists should discuss the various options with their patients, taking into account their preferences and tolerance, as well as access to equipment or exercise venues, in order to promote exercise as a primary treatment approach.[27] Strategies for improving adherence to therapeutic exercise, such as education, goal setting, monitoring, and feedback, may help maintain participation and optimize clinical benefits over the longer term.[6]
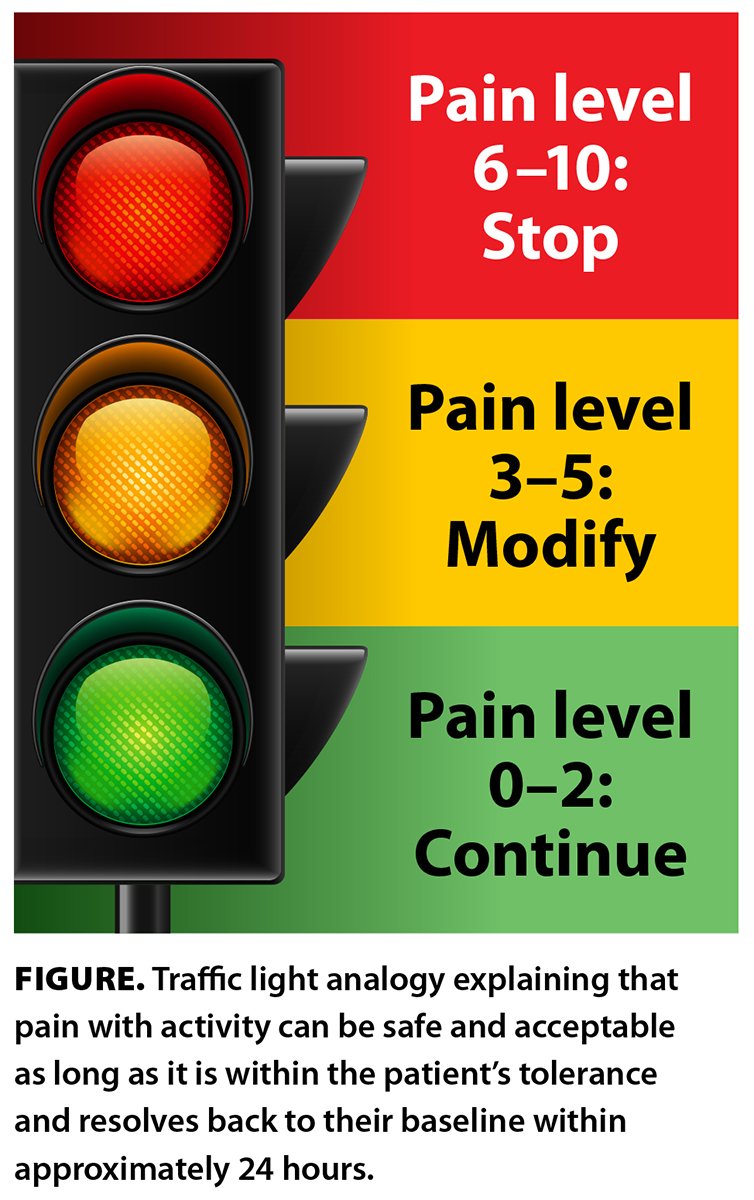 Although there is good evidence that patients with osteoarthritis benefit by staying active, there is little research on whether they should continue to participate in popular sports such as tennis, pickleball, downhill skiing, and cross-country skiing. Therefore, general advice on exercising within pain tolerance and monitoring pain levels/response over 24 hours can help determine whether a patient’s preferred activity is appropriate, given their symptomatology. Physiotherapists often use visual guides; a common one is the pain and activity traffic light [Figure]. This can help patients decide what is safe and acceptable for them when exercising and can reassure them that some discomfort with activity is normal and not damaging to the knee joint.
Although there is good evidence that patients with osteoarthritis benefit by staying active, there is little research on whether they should continue to participate in popular sports such as tennis, pickleball, downhill skiing, and cross-country skiing. Therefore, general advice on exercising within pain tolerance and monitoring pain levels/response over 24 hours can help determine whether a patient’s preferred activity is appropriate, given their symptomatology. Physiotherapists often use visual guides; a common one is the pain and activity traffic light [Figure]. This can help patients decide what is safe and acceptable for them when exercising and can reassure them that some discomfort with activity is normal and not damaging to the knee joint.
Biomechanical interventions
Biomechanical interventions include a broad range of apparatuses and appliances that are intended to improve patients’ function, relieve pain, and potentially reduce disease progression. The main mechanisms underlying these approaches are to reduce stress on the knee by redistributing load and to enhance joint stability by increasing proprioceptive input. For knee osteoarthritis, shoe inserts, walking aids, footwear, and braces (addressed by Sidhu and colleagues in Part 1 of this two-part theme issue) are of the most interest in the physiotherapy clinical practice.
Physiotherapists may recommend a trial of using shoe inserts and may assess for any symptomatic change at follow-up appointments. Evidence of the benefit of using shoe inserts, such as lateral wedged insoles, is mixed. For some patients, they can be a safe and low-cost orthosis option that may help symptoms, but they do not appear to improve the biomechanics of the knee.[28]
Compared with other biomechanical interventions, there is a dearth of research on using walking aids to manage knee osteoarthritis. However, the Arthritis Foundation website, National Institute for Health and Care Excellence guidelines, and Osteoarthritis Research Society International suggest that walking aids (e.g., canes, crutches, frames, wheeled walkers) are appropriate and effective and help increase independence and safety.[1,4] They can reduce mechanical loading through the knee, relieve pain, and improve function.[1] Thus, most guidelines recommended them as an option for patients with knee osteoarthritis. Physiotherapists can educate patients about how to use any walking aid correctly to help improve balance, reduce the risk of falling by widening the base of support, and reduce weight on lower-body joints.[29]
Adjunct therapies
Adjunct therapies have traditionally been a component of physiotherapeutic intervention for osteoarthritis. However, there is a lack of high-quality research on the additional benefits of using adjunct therapies such as heat or ice, low-level laser therapy, therapeutic ultrasonography, manual therapy, and acupuncture.[4,5,14] It has yet to be determined if any adjuncts have complementary effects when combined with education and exercise.
Anecdotally, many patients report benefits from using either heat or ice, and many international guidelines suggest their use can be beneficial for short-term pain management. There is evidence that self-administered heat and/or ice provides a mild improvement in pain, functional status, and quality of life. The use of heat or ice for pain relief may depend on personal preference and/or gender.[30]
The Osteoarthritis Research Society International guidelines recommend against using low-level laser therapy and ultrasonography, citing very low-quality evidence of their benefit in managing osteoarthritis.[4] However, there may be some value for the patient depending on their personal beliefs and preferences. The American College of Rheumatology recommends taking into account patient preferences regarding the use of ultrasonography.[14]
According to the National Institute for Health and Care Excellence, Osteoarthritis Research Society International, European Alliance of Associations for Rheumatology, and American College of Rheumatology guidelines, there is low-quality evidence that manual therapies such as massage, mobilization or manipulation, and passive range of motion provide additional benefit in treating knee osteoarthritis; therefore, their use should be considered only alongside therapeutic exercise.[1,4,5,14] The National Institute for Health and Care Excellence and the United States Bone and Joint Initiative both recognize the potential contributions that manual therapy can make to patient outcomes, given individual preferences, and they recommend considering using manual therapy, but only if it is combined with exercise.[1,7]
Research shows low-quality evidence in favor of using acupuncture to treat knee osteoarthritis. The Osteoarthritis Research Society International states that acupuncture is “an implausible biological mechanism”[4] and strongly recommends against its use. However, the American College of Rheumatology conditionally recommends its use when considering patient preferences.[14]
In summary, thermal modalities are recommended for knee osteoarthritis, therapeutic ultrasonography is not recommended for use, and there is insufficient evidence to provide a general recommendation for the use of acupuncture. According to the United States Bone and Joint Initiative, multiple organizations agree on many of the recommendations made for managing knee osteoarthritis. There is not a lack of quality guidelines but rather a deficit in dissemination and implementation of the recommendations.[31] Ideally, future efforts should focus on optimizing implementation in primary care settings, where most osteoarthritis care occurs.
Conclusion
Given the primary importance of education and exercise in managing osteoarthritis, physiotherapists are well suited to assisting general practitioners in managing all levels of arthritis through a continuum of care. The effects of these key management options compared with usual care or surgical procedures result in cost savings and improvement in quality of life. Physiotherapy should be considered as a safe and effective nonpharmacological intervention that can be used to manage knee osteoarthritis and enhance patients’ quality of life.
Competing interests
Ms Barber works in private practice at Envision Physiotherapy in Vancouver. Mr Jahanbani is a personal trainer at Elevate Training, Health, and Wellness in Vancouver.
This article has been peer reviewed.
 |
| This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. |
References
1. National Institute for Health and Care Excellence (NICE). Osteoarthritis in over 16s: Diagnosis and management. NICE Guideline, No. 226. London, UK: NICE, 2022. Accessed 22 March 2024. www.ncbi.nlm.nih.gov/books/NBK588843/.
2. Kopec JA, Heath AJ, Sayre EC, et al. Prevalence of joint-specific osteoarthritis and joint pain in British Columbia, Canada. Rheumatol Int 2022;42:1623-1628.
3. Cross M, Smith E, Hoy D, et al. The global burden of rheumatoid arthritis: Estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis 2014;73:1316-1322.
4. Bannuru RR, Osani MC, Vaysbrot EE, et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis Cartilage 2019;27:1578-1589.
5. Rausch Osthoff A-K, Juhl CB, Knittle K, et al. Effects of exercise and physical activity promotion: Meta-analysis informing the 2018 EULAR recommendations for physical activity in people with rheumatoid arthritis, spondyloarthritis and hip/knee osteoarthritis. RMD Open 2018;4:e000713.
6. Fransen M, Crosbie J, Edmonds J. Physical therapy is effective for patients with osteoarthritis of the knee: A randomized controlled clinical trial. J Rheumatol 2001;28:156-164.
7. National Institute for Health and Care Excellence (NICE). Osteoarthritis: Care and management. NICE Clinical Guidelines, No. 177. London, UK: NICE, 2020. Accessed 22 March 2024. www.ncbi.nlm.nih.gov/books/NBK568417/.
8. Superio-Cabuslay E, Ward MM, Lorig KR. Patient education interventions in osteoarthritis and rheumatoid arthritis: A meta-analytic comparison with nonsteroidal antiinflammatory drug treatment. Arthritis Care Res 1996;9:292-301.
9. Ackerman IN, Bucknill A, Page RS, et al. Preferences for disease-related education and support among younger people with hip or knee osteoarthritis. Arthritis Care Res 2017;69:499-508.
10. Bi X. Correlation of serum cartilage oligomeric matrix protein with knee osteoarthritis diagnosis: A meta-analysis. J Orthop Surg Res 2018;13:262.
11. Uthman OA, van der Windt DA, Jordan JL, et al. Exercise for lower limb osteoarthritis: Systematic review incorporating trial sequential analysis and network meta-analysis. BMJ 2013;347:f5555.
12. Slemenda C, Brandt KD, Heilman DK, et al. Quadriceps weakness and osteoarthritis of the knee. Ann Intern Med 1997;127:97-104.
13. Canadian Society for Exercise Physiology. Canadian 24-hour movement guidelines for adults aged 18–64 years: An integration of physical activity, sedentary behaviour, and sleep. Accessed 11 March 2023. https://csepguidelines.ca/guidelines/adults-18-64/.
14. Kolasinski SL, Neogi T, Hochberg MC, et al. 2019 American College of Rheumatology/Arthritis Foundation guideline for the management of osteoarthritis of the hand, hip, and knee. Arthritis Care Res 2020;72:149-162.
15. Burnet K, Kelsch E, Zieff G, et al. How fitting is F.I.T.T.?: A perspective on a transition from the sole use of frequency, intensity, time, and type in exercise prescription. Physiol Behav 2019;199:33-34.
16. Wellsandt E, Golightly Y. Exercise in the management of knee and hip osteoarthritis. Curr Opin Rheumatol 2018;30:151-159.
17. American College of Sports Medicine. Physical activity guidelines. Accessed 12 March 2023. www.acsm.org/education-resources/trending-topics-resources/physical-activity-guidelines/.
18. Raymond MJ, Bramley-Tzerefos RE, Jeffs KJ, et al. Systematic review of high-intensity progressive resistance strength training of the lower limb compared with other intensities of strength training in older adults. Arch Phys Med Rehabil 2013;94:1458-1472.
19. Lo GH, Vinod S, Richard MJ, et al. Association between walking for exercise and symptomatic and structural progression in individuals with knee osteoarthritis: Data from the Osteoarthritis Initiative cohort. Arthritis Rheumatol 2022;74:1660-1667.
20. White DK, Tudor-Locke C, Zhang Y, et al. Daily walking and the risk of incident functional limitation in knee osteoarthritis: An observational study. Arthritis Care Res (Hoboken) 2014;66:1328-1336.
21. Migliorini F, Marsilio E, Oliva F, et al. Elderly runners and osteoarthritis: A systematic review. Sports Med Arthrosc Rev 2022;30:92-96.
22. Lo GH, Musa SM, Driban JB, et al. Running does not increase symptoms or structural progression in people with knee osteoarthritis: Data from the osteoarthritis initiative. Clin Rheumatol 2018;37:2497-2504.
23. Song J-A, Oh JW. Effects of aquatic exercises for patients with osteoarthritis: Systematic review with meta-analysis. Healthcare (Basel) 2022;10:560.
24. Arthritis Foundation. Exercises to engage mind and body. Accessed 11 March 2023. www.arthritis.org/health-wellness/healthy-living/physical-activity/yoga/exercises-to-engage-mind-and-body.
25. GLA:D Canada. Results in Canada. Accessed 22 March 2024. https://gladcanada.ca/results.
26. Dell’Isola A, Jönsson T, Ranstam J, et al. Education, home exercise, and supervised exercise for people with hip and knee osteoarthritis as part of a nationwide implementation program: Data from the Better Management of Patients with Osteoarthritis Registry. Arthritis Care Res (Hoboken) 2020;72:201-207.
27. Kanavaki AM, Rushton A, Efstathiou N, et al. Barriers and facilitators of physical activity in knee and hip osteoarthritis: A systematic review of qualitative evidence. BMJ Open 2017;7:e017042.
28. Ferreira V, Machado L, Vilaça A, et al. Effects of tailored lateral wedge insoles on medial knee osteoarthritis based on biomechanical analysis: 12-week randomized controlled trial. Clin Rehabil 2021;35:1235-1246.
29. Arthritis Foundation. Physical therapies and devices. Accessed 20 March 2023. www.arthritis.org/health-wellness/treatment/complementary-therapies/physical-therapies/physical-therapies-and-devices.
30. Denegar CR, Schimizzi ME, Dougherty DR, et al. Responses to superficial heating and cooling differ in men and women with knee osteoarthritis. Physiother Theory Pract 2012;28:198-205.
31. Nelson AE, Allen KD, Golightly YM, et al. A systematic review of recommendations and guidelines for the management of osteoarthritis: The Chronic Osteoarthritis Management Initiative of the U.S. Bone and Joint Initiative. Semin Arthritis Rheum 2014;43:701-712.
Ms Barber is a registered physiotherapist and a member of the Canadian Physiotherapy Association, a fellow of the Canadian Academy of Manipulative Physiotherapy, and a Gunn IMS–certified physiotherapist working in private practice at Envision Physiotherapy in Vancouver. Mr Jahanbani is a kinesiologist and a member of the British Columbia Association of Kinesiologists. He is a personal trainer at Elevate Training, Health, and Wellness in Vancouver.
Corresponding author: Ms Tracy Barber, tracybarberphysio@gmail.com.
