Integrating planetary health into case-based learning for medical students
ABSTRACT
Background: Climate change is a health emergency, yet many medical schools provide minimal planetary health content in their undergraduate medical curriculum. This pilot project answered the global call to recognize the impacts of climate change on human health by creating a way to address the gap in the curriculum at the University of British Columbia.
Methods: A multidisciplinary team of students, academic leadership, medical educators, and planetary health experts integrated climate change concepts into case-based learning scenarios and created patient perspective videos to supplement the cases.
Results: Planetary health concepts were integrated into four cases on topics relevant to the British Columbia context. The cases focused on identifying vulnerable patients, addressing risk factors, and managing climate-related illness. A unique feature of this pilot project was the involvement of near peers to edit the cases to target the appropriate level of complexity for the learners.
Conclusions: This pilot project demonstrates practical, strategic integration of climate change education into existing curricula. This collaborative approach, using multidisciplinary teams and patient perspectives, offers a model to prepare future clinicians for the impacts of climate change.
A pilot project demonstrates how climate change education can be integrated into an existing medical school curriculum.
Climate change is a global health emergency, with over 200 scientific journals coming together to call for action from political leaders and health professionals to recognize the impacts of climate change on human health.[1] Medical schools are an appropriate place for students to reflect on their roles and responsibilities to provide care in the era of climate change.[2] As highlighted in a 2019 CMAJ news story, medical students across Canada are calling for greater emphasis on planetary health in medical education, yet medical curricula often lag in incorporating this content.[3] According to one report, climate change is taught in only 15% of medical schools worldwide, and 34% of schools have no aspects of the involvement of climate in health included in either the mandatory or informal curriculum.[4] This article showcases a practical approach to curricular reform from the Faculty of Medicine at the University of British Columbia. This initiative’s process and lessons provide an example for other medical educators to apply when enhancing climate change education in their programs.
Background
The UBC Faculty of Medicine has been British Columbia’s main medical school for over 70 years. In keeping with medical schools across Canada, a key component of the UBC MD curriculum in years 1 and 2 is case-based learning, during which students work through a weekly patient case related to a specific topic in a small group format.[5] This teaching format emphasizes problem-solving, critical thinking, and student collaboration to address health through a biopsychosocial model.[6] In the UBC curriculum, cases spiral onto one another, and each topic is revisited, with increasing complexity, multiple times throughout years 1 and 2.[7]
Methods
We convened a multidisciplinary team of medical students and clinical faculty members with expertise in academic leadership, medical education, and planetary health to integrate climate change concepts into existing case-based learning content, focusing on identifying vulnerable patients, addressing risk factors, and managing climate-related illness. During this pilot phase, our team focused on cases of chronic obstructive pulmonary disease (COPD), kidney disease, geriatric health, and mental health. These cases were chosen, in consultation with the respective case leads, because there is strong evidence that the subject areas are impacted by climate change and are acutely relevant in British Columbia due to increased critical climate events in recent years (e.g., forest fires, heat waves). The integration was done in three stages:
- Conducting a literature review. A medical student (A.G.) reviewed the planetary health literature related to the selected cases, with support from the planetary health expert (V.S.). Articles were chosen based on pathophysiology and common presentations for each topic, alongside specific impacts of climate change, forest fires, and increasing temperatures.
- Editing the case-based learning content. The literature review informed the modification of case-based learning prompts and questions to integrate climate change considerations into health care and patient outcomes. For rigor, modifications were discussed and approved by the week’s leads for each case. Selected references from the review were added as recommended reading for each week.
- Incorporating patient perspectives. A medical student (E.W.) collaborated with patient partners to develop short videos, centred on patient experiences, illustrating real-life impacts of climate change on an individual’s health. The videos were included in the cases.
Results: The selected cases
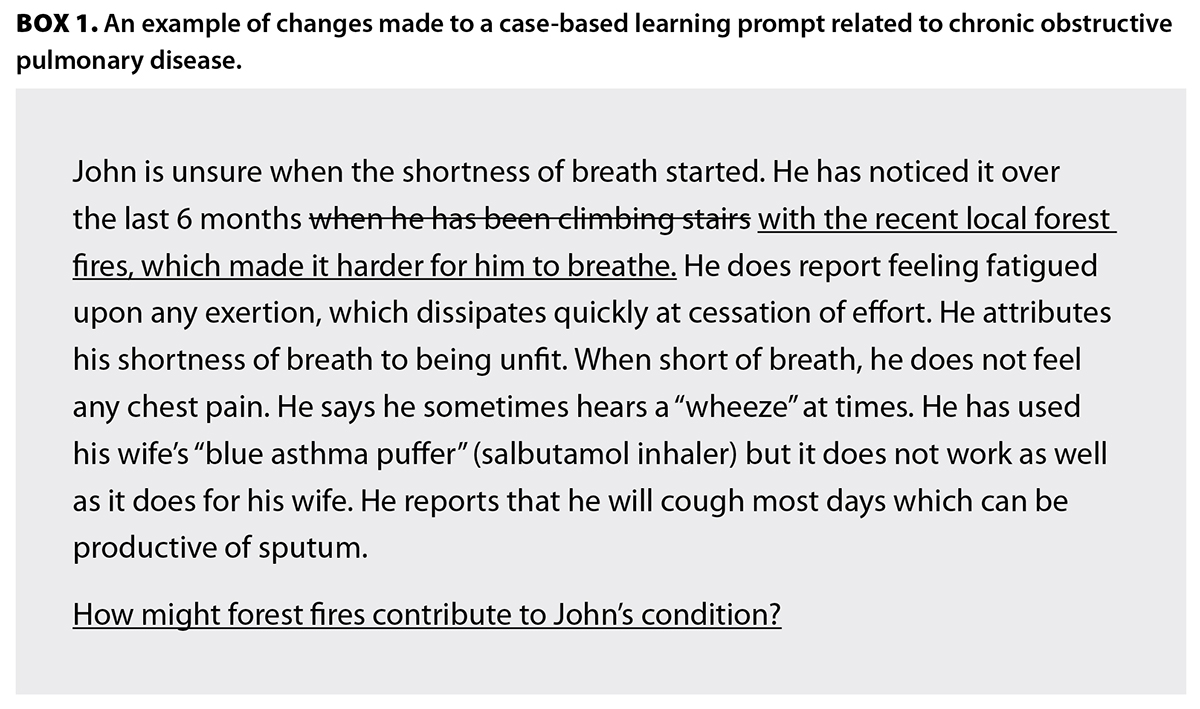 Chronic obstructive pulmonary disease
Chronic obstructive pulmonary disease
In 2023, BC experienced the most destructive forest fire season in recent history, involving nearly 3 million hectares of land.[8] Forest fires affect air quality by increasing acute exposure to airborne pollutants, including particulate matter and carbon monoxide,[9] which in turn leads to adverse outcomes among patients with respiratory diseases. Chronic increases in particulate matter increase the likelihood of developing COPD in adults[10] and asthma in children.[11] Acute exposure to poor air quality also increases emergency room visits, hospital admissions, and mortality among patients with COPD.[12]
This was addressed in the UBC curriculum, as shown in Box 1, in a case where a patient had a COPD exacerbation. The exacerbating factor was adjusted in this case to be an environmental issue, rather than exertion. Students were also asked to discuss how forest fires could be contributing to the patient’s condition, allowing students to explore the impact of critical climate events on human health.
This case was paired with an embedded video highlighting a real patient’s experience of the 2003 Okanagan Mountain Park wildfire, which resulted in hospitalization and significant worsening of her asthma disease burden. Students watched the video as a group and received prompting questions to reflect on how climate change impacts quality of life.
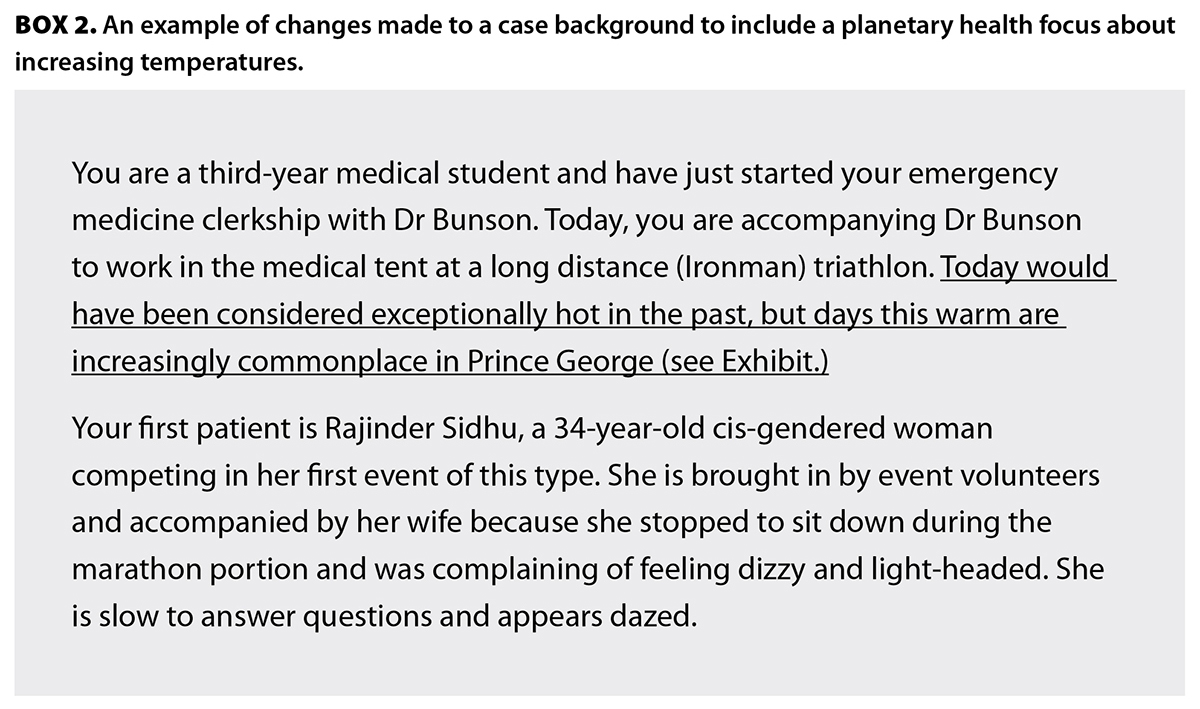 Kidney disease
Kidney disease
Rising average temperatures in the context of climate change worsen both acute and chronic kidney disease through increased inflammation and decreased renal blood flow.[13] Individuals performing physically demanding work outdoors, such as farmers, construction workers, plantation workers, and miners, are more likely to develop this “heat stress nephropathy.”[13] Exercise in intense heat, particularly without acclimation, can cause additional stress on the kidneys through two pathways. First, higher temperatures require diversion of blood to the skin for heat dissipation, with compensatory restriction of blood flow to the kidneys. Second, increased temperatures require increased sweating for thermoregulation, resulting in an increased risk for volume and electrolyte depletion.[14]
In this case, the patient developed an electrolyte disturbance after participating in a triathlon during a heat wave. The case was modified to highlight the increasing temperatures in Prince George and the exceptionally hot weather on the day of the event [Box 2].
Students were asked to research the impacts of climate change on kidney function and come to the session prepared to discuss. Students were also asked to brainstorm ways that event organizers could have better prepared for athletes who were suffering from heat stress, placing an emphasis on prevention and harm reduction.
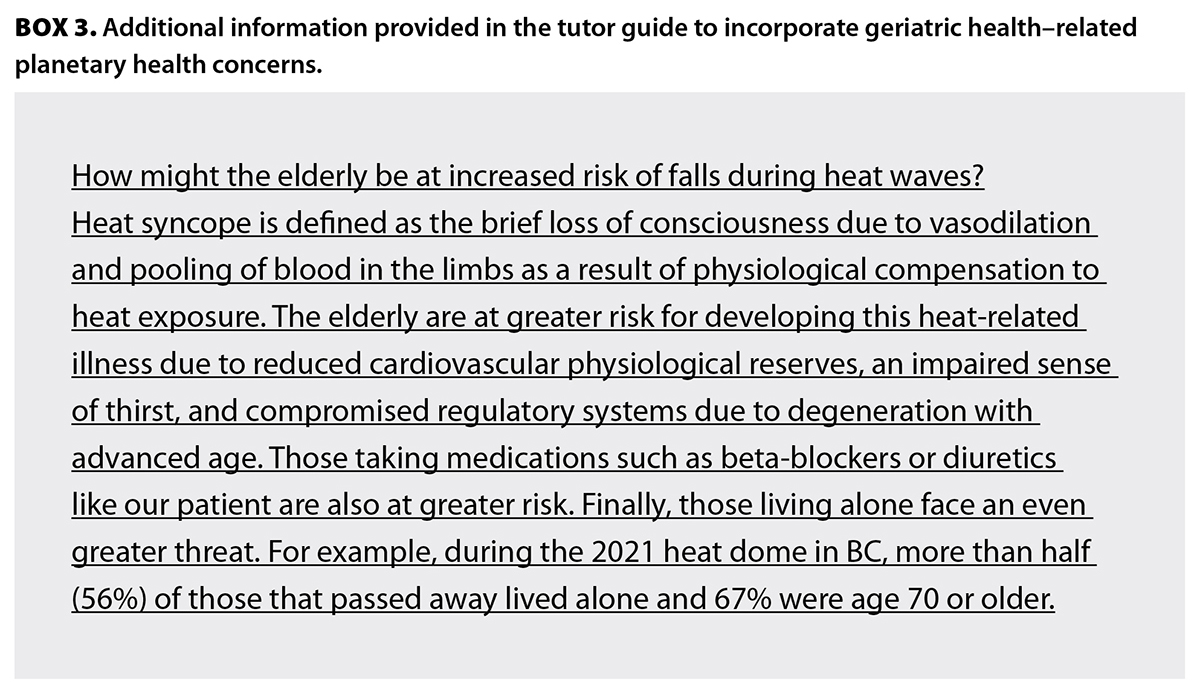 Geriatric health
Geriatric health
Elderly populations are increasingly vulnerable to the effects of climate change due to higher rates of chronic disease, greater sensitivity to heat, and increased use of medications that impair the ability to feel thirst, sweat, and thermoregulate.[15] This was especially evident during the 2021 heat dome in BC, where record temperatures were seen in many parts of the province over several days.[16] According to the coroner’s report, 619 deaths were attributed to this extreme weather event; 90% of those who died were over 60 years of age, and two-thirds were individuals with chronic illnesses that could impact mobility, such as heart failure, arthritis, and Parkinson disease.[16] Elderly individuals are also at increased risk of developing heat-related illnesses like heat syncope, which could increase the risk of falls in this population.[17]
Incorporating planetary health concepts into osteoporosis week highlights the downstream impacts of climate change on conditions not traditionally associated with planetary health. In this case, an elderly patient falls and presents to the emergency department with a fracture. She is subsequently diagnosed with osteoporosis. The original cause of the fall was tripping over a carpet; it was changed to dehydration and heat syncope, leading to the fall. Students were asked to prepare to discuss how elderly patients might be at increased risk of falls during heat waves. The accompanying tutor guide addresses heat syncope and physiological responses to heat that put elderly patients at greater risk. Box 3 shows the additional information provided in the tutor guide for this case.
Additional risk factors, such as lack of air conditioning, low socioeconomic status, and limited social supports, are emphasized throughout the case.
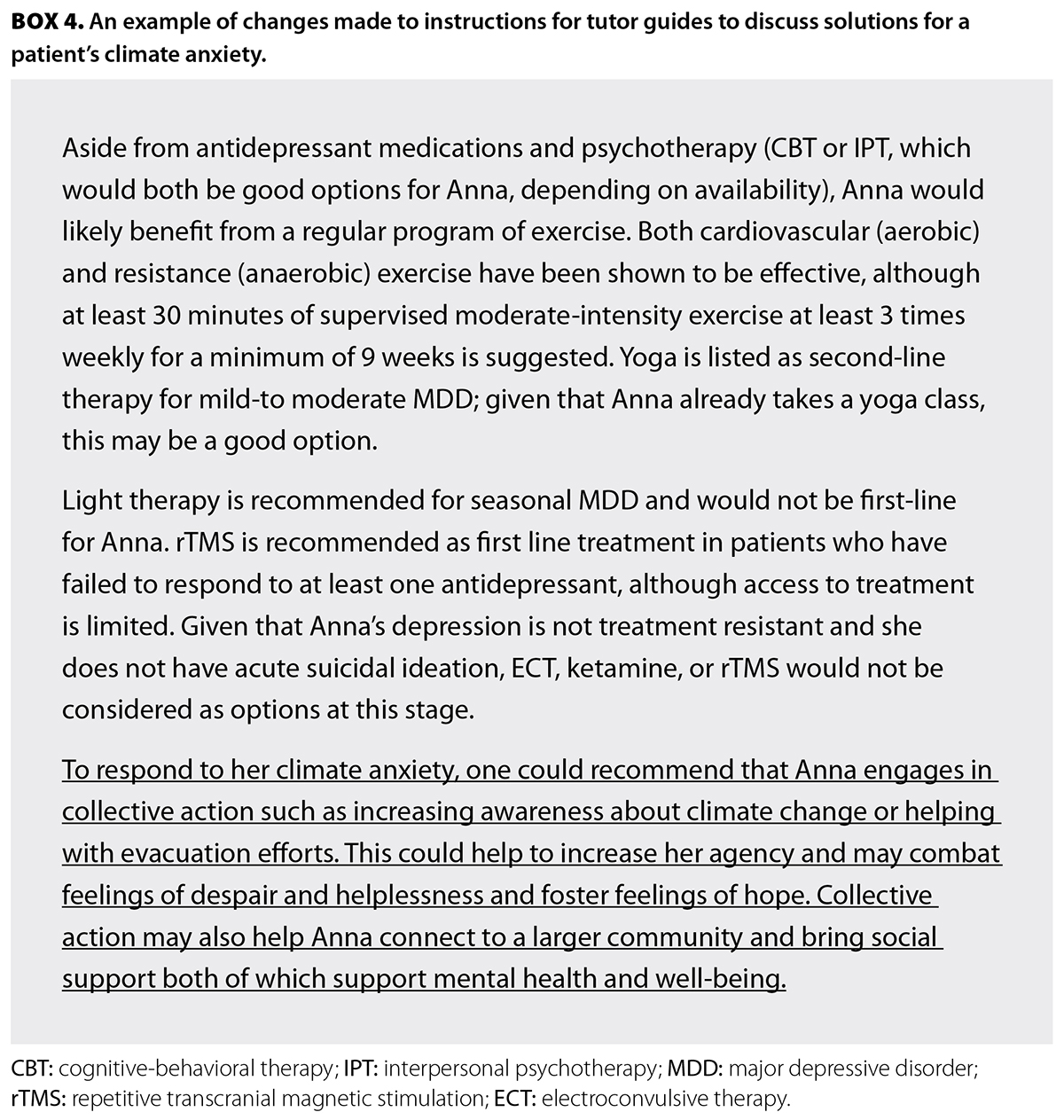 Mental health
Mental health
Climate change impacts mental health, contributing to conditions like climate change anxiety, both physical and mental symptoms, and apprehension about the future in response to climate change.[18] This may worsen during emergency weather events, such as the 2021 heat dome, which exacerbated climate change anxiety in British Columbians.[18] Exposure to natural disasters is also strongly associated with high psychological distress, including posttraumatic stress disorder and depression.[19] Individuals can also experience climate change anxiety even when not directly involved in a climate disaster.[20]
The case for this week was modified so the patient’s anxiety disorder centred on wildfires and warming temperatures in her area. In addition to treating the patient with an antidepressant, psychotherapy, and other lifestyle measures, the case had tutors discuss evidence-based strategies that can be used to address climate change anxiety, such as participating in community efforts to tackle climate change, including rallies, cleanup efforts, and community gardens [Box 4].[21] While raising awareness of the psychological effects of climate change can be triggering, presenting this information through a collective-action lens may combat feelings of despair and hopelessness, and instead foster hope.[22,23]
This case was accompanied by a patient video that highlights a young woman’s experience with climate anxiety living in Vancouver. Students were asked to review the video independently and come to the sessions prepared to discuss and reflect on her experiences.
Discussion of limitations and solutions
Key barriers in this project included having to balance the integration of climate change education with an already dense preclinical curriculum and contending with a decentralized weekly block structure. Similar concerns were raised at McMaster University when it attempted to incorporate climate change education into its medical curriculum.[25]
To overcome the dense curriculum barrier, the new material was woven into existing elements of the curriculum rather than being added as new elements focused solely on planetary health.[26] Although the siloed, decentralized structure of the program made it challenging to implement changes through a centralized process, this was addressed through direct communication and collaboration between the leads of each individual week and the planetary health team. One of the recommendations made by the group at McMaster University was to have designated individuals tasked with integrating climate change into the curriculum to ensure continuity.[25] This approach situates learning in a relevant context, endorses climate change health concerns, and promotes permanence of the curriculum change.[26]
Conclusions
While integrating climate change education into a demanding medical curriculum presents obstacles, the UBC experience demonstrates that strategic, collaborative, and creative approaches can effectively address the challenges and equip graduates to be environmentally responsible clinicians prepared for the health impacts of climate change.
Competing interests
None declared.
Acknowledgments
The authors gratefully acknowledge funding and support from UBC Sustainability, which made this initiative possible. They also deeply appreciate the invaluable contributions from their patient partners, whose lived experiences and insights shaped the relevance and impact of the content. Special thanks to the UBC MD Undergraduate Education course directors for their collaboration and to Mr Stephen Gillis from the audiovisual department for his support with video creation and filming.
This article has been peer reviewed.
 |
| This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. |
References
1. Abbasi K, Ali P, Barbour V, et al. Time to treat the climate and nature crisis as one indivisible global health emergency. BMJ 2023;383:p2355. https://doi.org/10.1136/bmj.p2355.
2. Wellbery C, Sheffield P, Timmireddy K, et al. It’s time for medical schools to introduce climate change into their curricula. Acad Med 2018;93:1774-1777. https://doi.org/10.1097/ACM.0000000000002368.
3. Mercer C. Medical students call for more education on climate change. CMAJ 2019;191:E291-E292. https://doi.org/10.1503/cmaj.109-5717.
4. Galway LP, Burkhardt R, Berger P, Cameron E. Climate change in medical school curricula: A status report. Lakehead University. April 2021. Accessed 12 April 2025. www.nosm.ca/wp-content/uploads/2021/08/LU-Climate-Change-in-Medical-School-Curricula-A-Status-Report_FINAL.pdf.
5. MD Undergraduate Program, UBC Faculty of Medicine. Curriculum. Accessed 25 August 2024. https://mdprogram.med.ubc.ca/about/curriculum/.
6. Werner A, Werner EA, Mullan PB. Teaching students to identify psychosocial cues in problem-based learning cases. Acad Psychiatry 1997;21:86-90. https://doi.org/10.1007/BF03341903.
7. Harden RM. What is a spiral curriculum? Med Teach 1999;21:141-143. https://doi.org/10.1080/01421599979752.
8. BC Wildfire Service. Wildfire averages. Last updated 8 July 2025. Accessed 6 March 2025. www2.gov.bc.ca/gov/content/safety/wildfire-status/about-bcws/wildfire-statistics/wildfire-averages.
9. Sapkota A, Symons JM, Kleissl J, et al. Impact of the 2002 Canadian forest fires on particulate matter air quality in Baltimore city. Environ Sci Technol 2005 39:24-32. https://doi.org/10.1021/es035311z.
10. Ling S, van Eeden SF. Particulate matter air pollution exposure: Role in the development and exacerbation of chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis 2009;4:233-243. https://doi.org/10.2147/COPD.s5098.
11. Dhingra R, Keeler C, Staley BS, et al. Wildfire smoke exposure and early childhood respiratory health: A study of prescription claims data. Environ Health 2023;22:48. https://doi.org/10.1186/s12940-023-00998-5.
12. Government of British Columbia. Chronic obstructive pulmonary disease (COPD): Diagnosis and management. Revised 17 January 2025. Accessed 12 April 2025. www2.gov.bc.ca/gov/content/health/practitioner-professional-resources/bc-guidelines/copd.
13. Glaser J, Lemery J, Rajagopalan B, et al. Climate change and the emergent epidemic of CKD from heat stress in rural communities: The case for heat stress nephropathy. Clin J Am Soc Nephrol 2016;11:1472-1483. https://doi.org/10.2215/CJN.13841215.
14. Schlader ZJ, Hostler D, Parker MD, et al. The potential for renal injury elicited by physical work in the heat. Nutrients 2019;11:2087. https://doi.org/10.3390/nu11092087.
15. Błeszyńska E, Wierucki Ł, Zdrojewski T, Renke M. Pharmacological interactions in the elderly. Medicina (Kaunas) 2020;56:320. https://doi.org/10.3390/medicina56070320.
16. BC Coroners Service Death Review Panel. Extreme heat and human mortality: A review of heat-related deaths in B.C. in summer 2021. 7 June 2022. Accessed 12 April 2025. www2.gov.bc.ca/assets/gov/birth-adoption-death-marriage-and-divorce/deaths/coroners-service/death-review-panel/extreme_heat_death_review_panel_report.pdf.
17. Sorensen C, Hess J. Treatment and prevention of heat-related illness. N Engl J Med 2022;387:1404-1413. https://doi.org/10.1056/NEJMcp2210623.
18. Bratu A, Card KG, Closson K, et al. The 2021 Western North American heat dome increased climate change anxiety among British Columbians: Results from a natural experiment. J Clim Change Health 2022;6:100116. https://doi.org/10.1016/j.joclim.2022.100116.
19. Beaglehole B, Mulder RT, Frampton CM, et al. Psychological distress and psychiatric disorder after natural disasters: Systematic review and meta-analysis. Br J Psychiatry 2018;213:716-722. https://doi.org/10.1192/bjp.2018.210.
20. Clayton S, Manning C, Krygsman K, Speiser M. Mental health and our changing climate: Impacts, implications, and guidance. American Psychological Association, Climate for Health, ecoAmerica. March 2017. Accessed 9 April 2025. https://climahealth.info/resource-library/mental-health-and-our-changing-climate-impacts-implications-and-guidance/.
21. Schwartz SEO, Benoit L, Clayton S, et al. Climate change anxiety and mental health: Environmental activism as buffer. Curr Psychol 2022;42:16708-16721. https://doi.org/10.1007/s12144-022-02735-6.
22. Ramírez-López AS, Rosetti MF, Poma A. Gender, exposure to news, knowledge about climate change, and prosociality predict climate anxiety scores in Mexican students. Ecopsychology 2023;15:184-192. https://doi.org/10.1089/eco.2022.0049.
23. Asgarizadeh Z, Gifford R, Colborne L. Predicting climate change anxiety. J Environ Psychol 2023;90:102087. https://doi.org/10.1016/j.jenvp.2023.102087.
24. McLeod S. Zone of proximal development. Simply Psychology. Accessed 9 April 2025. www.simplypsychology.org/zone-of-proximal-development.html.
25. Hansen M, Rohn S, Moglan E, et al. Promoting climate change issues in medical education: Lessons from a student-driven advocacy project in a Canadian medical school. J Clim Change Health 2021;3:100026. https://doi.org/10.1016/j.joclim.2021.100026.
26. Maxwell J, Blashki G. Teaching about climate change in medical education: An opportunity. J Public Health Res 2016;5:673. https://doi.org/10.4081/jphr.2016.673.
Mr Gangji and Ms Willis are medical students in the undergraduate medical program, University of British Columbia. Dr Yee is a hematologist and clinical associate professor in the Division of Hematology, Department of Medicine, UBC. Dr Gil-Mohapel is director of curriculum for undergraduate medical education in the undergraduate medical program and a lecturer in the Department of Family Practice and the Division of Neurology, Department of Medicine, UBC. She is also a teaching faculty member in the Division of Medical Sciences, University of Victoria. Dr Stoynova is a clinical assistant professor in the Department of Medicine, UBC, and a general internist in the Division of Internal Medicine, Island Health.
Corresponding author: Mr Ali Raza Gangji, amoham14@student.ubc.ca.

