Review Articles
How to approach the diagnosis of knee osteoarthritis
ABSTRACT: Knee osteoarthritis, a prevalent chronic disease, results from the loss of articular cartilage within the knee joint and is the leading cause of knee pain in adults. Early detection, lifestyle modifications, and patient education can improve patients’ quality of life, curb office visits for knee pain, and avert unnecessary imaging, interventions, and specialist referrals. In most patients, diagnosis can be established in the family practice setting based on a comprehensive pain history and physical examination. Standing X-rays of the knee joints are the gold standard for confirming the diagnosis. If imaging is required, radiography should be the first modality employed. If there is suspicion of an underlying infectious or inflammatory cause, further testing or referral to a specialist, such as an orthopaedic surgeon or rheumatologist, may be warranted. During the early stages of osteoarthritis, patients can be encouraged to undertake low-impact exercises and adopt a balanced diet to facilitate weight loss. This can ease the load on affected joints, strengthen the muscles that support the joints, improve mobility, and reduce pain. Educating patients about their condition can improve their ability to cope with the disease, enhance their adherence to treatment plans, and ultimately result in better clinical outcomes. Patients who are more knowledgeable about their condition experience less anxiety and a greater sense of control, which leads to better health outcomes.
Knee osteoarthritis is the leading cause of knee pain in adults. Family physicians can rely on a combination of patient history, physical examination, and standing knee X-rays to successfully diagnose it in the office.
Knee osteoarthritis, the predominant cause of chronic knee pain, often leads patients to consult their family practitioner. This complex joint disease is characterized by cartilage loss, reactive bone formation, subchondral cystic changes, joint deformity, and disruption of surrounding soft tissues, and manifests primarily as activity-related pain and functional limitation. Establishing a diagnosis and offering guidance on the anticipated clinical trajectory can enhance patients’ comprehension of their condition, curb office visits for knee pain, and avert unnecessary interventions such as indiscriminate physiotherapy and massage therapy in cases of unclear diagnosis. This article presents a systematic approach to recognizing and diagnosing knee osteoarthritis, thereby minimizing unwarranted testing.
Risk factors
Knee osteoarthritis affects approximately 40% of adults over the age of 60, and age over 50 years is the most significant risk factor.[1] Other risk factors include female sex, obesity, and history of knee malalignment or injury.[2,3] While the evidence concerning the influence of recreational activities on knee osteoarthritis risk is varied, it is improbable that such activities, provided they do not result in substantial joint injury, contribute to the onset of this condition.[3,4]
Causes
Knee osteoarthritis can be both primary and secondary.[5] As individuals age, the quantity of synovial fluid diminishes and the cartilage thins, leading to the onset of primary osteoarthritis. Patients with predisposing conditions may experience early or premature osteoarthritis due to secondary factors. Potential causes of secondary knee osteoarthritis include:
- Trauma, such as cruciate ligament injuries, intra-articular fractures, and extra-articular deformities.
- Crystalline arthritis (gout or calcium pyrophosphate deposition disease–related arthritis).
- Avascular necrosis.
- Metabolic diseases (e.g., ochronosis).
- Intra-articular infection.
- Inflammatory arthritis (e.g., rheumatoid arthritis, psoriatic arthritis).
- Iron overload (hemochromatosis).
- Hemophilia (recurrent hemarthrosis).
- Neoplasms, such as intra-articular tenosynovial giant cell tumors.
The bony remodeling associated with osteoarthritis leads to increased friction and pressure points within the knee joint, which precipitates pain and ultimately reduces mobility and flexibility. The multifaceted nature of this pain results from the loss of normal subchondral bone protection provided by articular cartilage and the exposure of the densely nerve-supplied subchondral bone, and from synovitis and inflammatory responses. However, the exact mechanisms have not been fully elucidated. There is no consistent correlation among knee osteoarthritis patients in terms of the degree of fluid and cartilage loss, bony changes, and pain.[5] Consequently, a patient’s level of pain does not always align with the severity of radiological changes, and radiological changes may not consistently correspond to actual pathological alterations.
Diagnosis
In most patients, the diagnosis of knee osteoarthritis is established using a combination of history and focused examination. Standing X-rays of the knee joints are the gold standard for confirming the diagnosis.[3] A comprehensive pain history, including the onset, location (i.e., left, right, or bilateral knee pain that is anterior, medial, or lateral), and quality of the pain, should be elicited.[5-7] Clinicians should pay close attention to the onset and severity of pain symptoms, the presence of any exacerbating or relieving factors, and the patient’s current level of functional activity. Additionally, it is essential to ask about any history of knee injuries or surgeries, preceding trauma, or instances of warmth or swelling in other peripheral joints.
Characteristic symptoms
Knee osteoarthritis pain is generally characterized as dull, either localized to a specific compartment or widespread, exacerbated by weight-bearing and joint movement, and eased with rest. Patients with patellofemoral osteoarthritis usually report a gradual onset of anterior knee pain, especially during activities that strain the knee in flexion, such as stair climbing, squatting, or rising from a seated position. Subjective stiffness often subsides in less than 30 minutes. Pain associated with knee osteoarthritis typically improves with rest, analgesics, and anti-inflammatory medication. Patients may also note a sensation of fullness or swelling at the back of the knee and a loss of extension, potentially indicating a related popliteal (Baker) cyst. It is critical to clarify that a Baker cyst does not cause pain, and its removal will not alleviate symptoms, a common misunderstanding among patients.[8]
Pain from osteoarthritis typically escalates in severity gradually over months to years, but patients can present at any stage of their disease. In the early or mild phases, pain is sporadic and predictable and has minimal impact on daily activities. Those with moderate osteoarthritis may endure unpredictable pain, possibly linked with knee locking or buckling, which could disrupt daily activities such as walking, bending, squatting, and stair climbing. In severe or advanced osteoarthritis, a constant dull pain is the norm, with occasional episodes of high-intensity pain limiting activities. Over time, patients may experience diminished functionality, including restricted joint movement, reduced ability to walk, and associated muscle weakness. In the long term, knee osteoarthritis can result in fatigue, sleep disturbances, and even depression.[8] Table 1 summarizes symptoms of early, moderate, and advanced knee osteoarthritis.
Physical examination
A physical examination should begin with an observation of lower limb alignment and gait.[9] An antalgic, or pain-induced, gait is characterized by a shorter stance phase and possibly reduced stride length on the affected side. When the patient is standing, examine both knees for deformities such as genu varum (bowleg deformity) or genu valgum (knock-knee deformity), which are indicative of more advanced osteoarthritis. Additionally, look for swelling in the popliteal region, which may suggest the presence of a Baker cyst.
With the patient lying supine on the examination table, conduct a thorough examination of the knee. The skin should be fully exposed to assess for any changes, including scars, erythema, ecchymosis, previous surgical marks, or skin conditions such as psoriasis. Examine the medial and lateral parapatellar fossae for swelling; although these areas may be obscured by adipose tissue, effusions, or bony remodeling, comparing them visually to the opposite knee may be informative. Examination for quadriceps muscle atrophy, which may signal chronic or more advanced pathology, should also be considered.
Divide palpation of joint lines and soft tissue structures into assessments of medial, midline, and lateral structures. With the knee flexed at 90 degrees, palpate the medial and lateral joint lines for tenderness or osteophytes (bony prominences). Patellar crepitus can be identified by holding the patella and passively flexing and extending the knee. The movement of the patella can be examined by pressing it medially and laterally; limited or painful movement could suggest patellofemoral osteoarthritis. Alternatively, patellofemoral disease may be detected by pressing the patella against the femoral condyles while the leg is extended and looking for signs of pain or discomfort.
Evaluate knee joint function by assessing range of motion and strength. Active knee flexion can be measured by asking the patient to bring their heel toward their buttock. The typical range of knee flexion for individuals with normally sized extremities is approximately 150 degrees, but flexion over 130 degrees would generally be considered normal for most individuals. If active range of motion is restricted, evaluate passive range of motion as well. Measure knee flexion strength through isometric strength testing with the patient lying supine. Stabilize the knee at a 90-degree angle with one hand, extend the leg with the other, and ask the patient to resist the movement. Have the patient straighten the leg, and evaluate extension by checking for a 180-degree angle. Any degree of flexion contracture is abnormal. Test the strength of knee extension by pushing against the patient’s leg and asking them to resist. Last, examination of the ipsilateral hip and lumbar spine is essential to check for pain that could be referred to the knee from the lower back or hip.
Special maneuvers
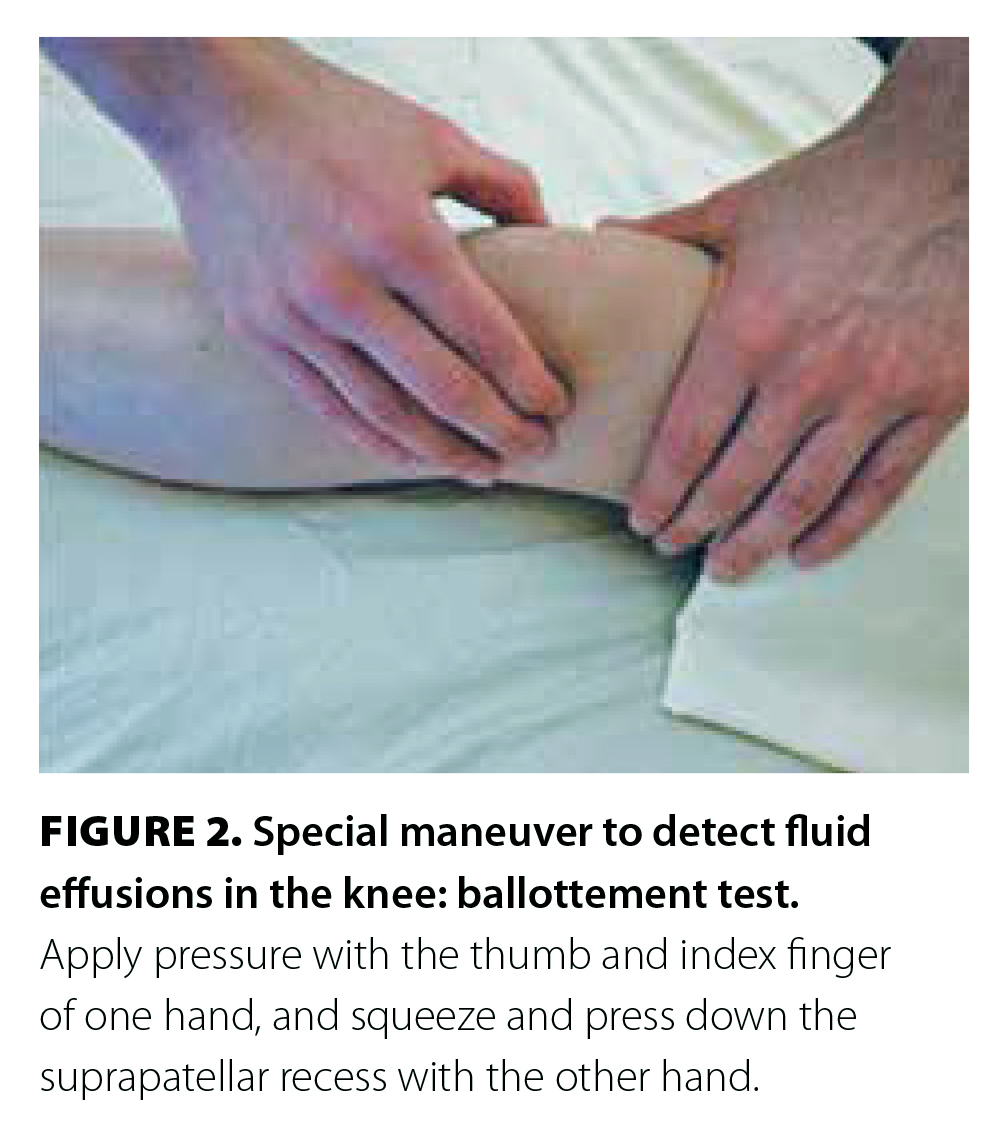
If there is suspicion of fluid effusions in the knees, further evaluation can be carried out using methods such as the fluid wave (for small effusions), ballottement (for moderate effusions), and patellar tap (for large effusions).[9] Perform the milking test for fluid wave or bulge sign in small effusions by applying firm pressure on the medial knee and sweeping your hand proximally along the medial side of the knee to push fluid into the lateral suprapatellar recess [Figure 1]. Then swiftly sweep your hand along the lateral knee and observe the medial fossa to detect whether a bulge forms.
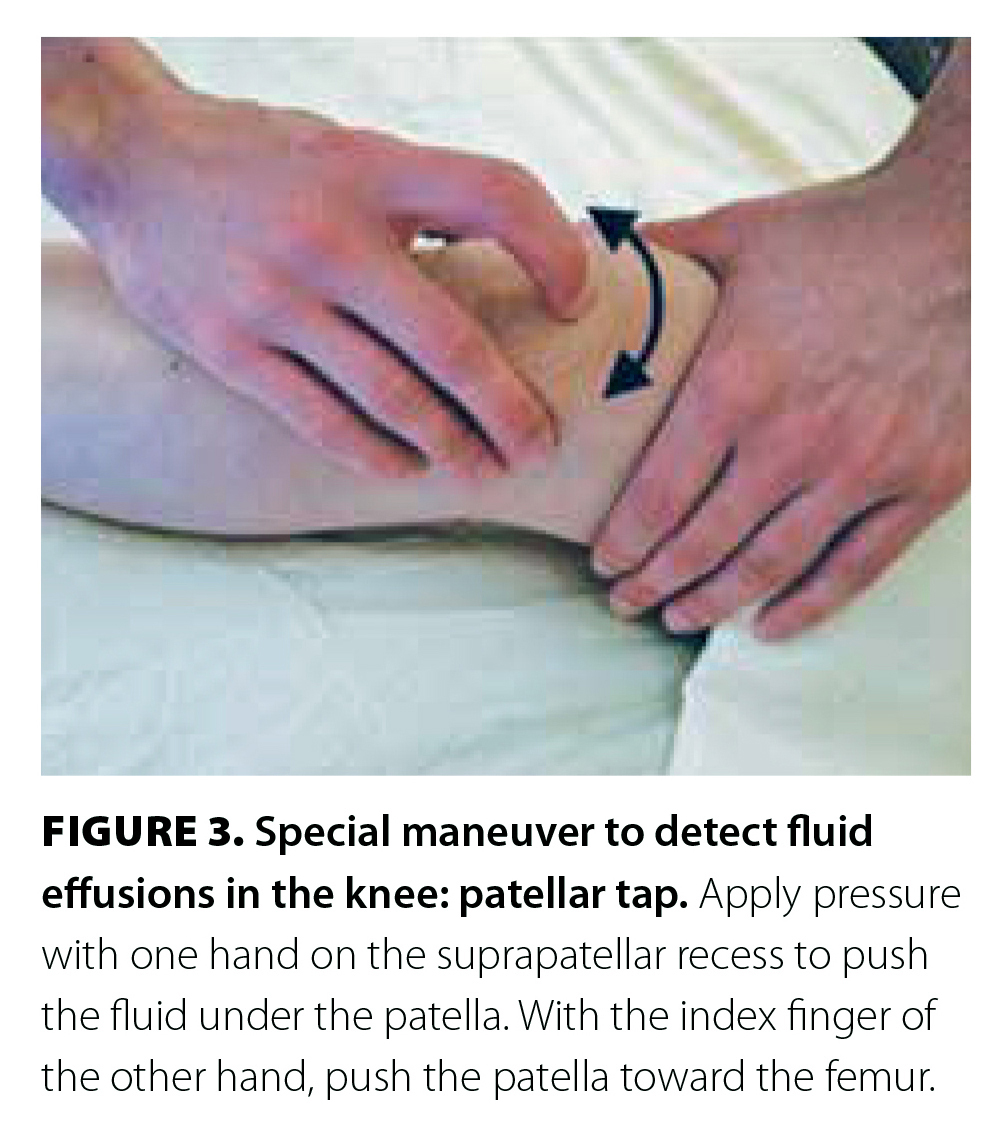
For moderate to large effusions, perform the ballottement test by cupping the thumb and fingers of one hand on either side of the patella and placing your other hand on the suprapatellar recess [Figure 2]. Apply firm pressure down above the patella; in cases of moderate effusions, fluid will form under your fingers and push them outward.
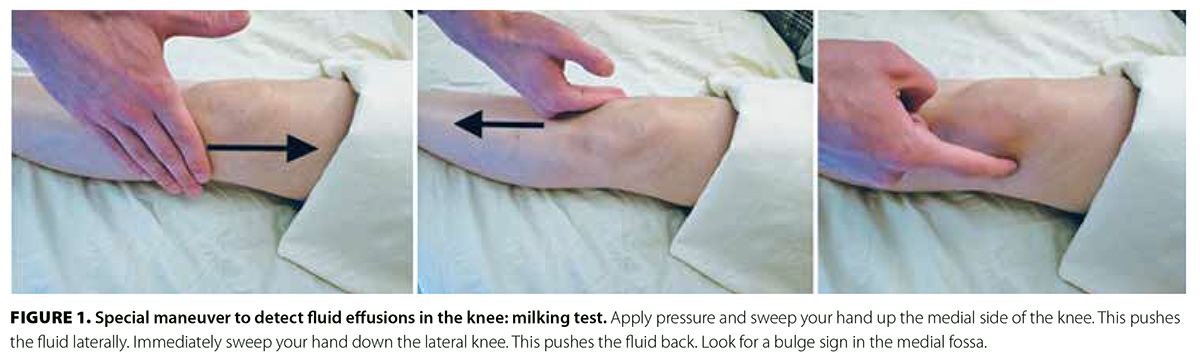
For large effusions, perform the patellar tap by placing one hand over the suprapatellar recess and applying pressure to displace fluid under the patella [Figure 3]. Then use a finger from the other hand to press the patella downward toward the femur. The patella should tap the femur and bounce back up to hit the finger.
 |
 |
Red flags warranting additional testing or referral
If there is any suspicion of an underlying infectious or inflammatory cause, further testing or referral to a specialist may be warranted. A warm or swollen knee could suggest inflammatory or septic arthritis, which necessitates further evaluation via arthrocentesis. Synovial fluid should typically be analyzed for cell count, differential, culture with Gram stain, and crystal examination. If infection is strongly suspected—such as in patients with fever, immunosuppression, or a history of intravenous drug use—additional tests, including complete blood count, C-reactive protein, and blood culture, are recommended. If there are concerns about inflammatory arthritis, a referral to a rheumatologist or orthopaedic surgeon may be advisable.
It is recommended to refer the patient to a rheumatologist if there are:[6]
- Risks of inflammatory arthritis.
- Small and large joint polyarthritis symptoms.
- Systemic symptoms such as weight loss or fatigue.
- Nonarticular symptoms, including rash, inflammatory bowel disease, or psoriasis.
Referral to an orthopaedic surgeon is recommended for patients with:
- Reduced effectiveness of pain management.
- Significantly reduced joint mobility that impacts daily activities.
- Failure of pain medication and treatment programs.
Imaging
Contemporary clinical practice guidelines suggest that knee osteoarthritis can be diagnosed without MRI in individuals over 45 years of age who present with activity-related joint pain, morning stiffness lasting less than 30 minutes, crepitus on active motion, and bony enlargement, provided there is no discernible warmth in the joint.[10] Deformity, instability, periarticular or joint-line tenderness, and pain with patellofemoral compression are additional characteristics that could exist.[3] Atypical characteristics such as a history of trauma, extended morning stiffness in the joint, rapid symptom progression, or the presence of a warm, swollen joint may indicate alternative or concurrent diagnoses. Consideration should be given to important differential diagnoses such as gout, other inflammatory arthritides (such as rheumatoid arthritis), septic arthritis, and malignancies causing bone pain. If a palpable effusion is detected, aspiration and analysis of the synovial fluid can aid in excluding septic arthritis, identifying the presence of urate or calcium pyrophosphate crystals, and ruling out other inflammatory arthritides.
Once knee osteoarthritis is suspected, its diagnosis should be confirmed using standing plain X-ray.[11] If imaging is required, radiography should be the first modality employed.
Conventional radiographs can expose characteristics of osteoarthritis in the affected joints, including joint space narrowing due to cartilage loss. In more advanced stages of knee osteoarthritis, radiographic findings may reveal subchondral cysts, sclerosis, bone spurs, and misaligned joint surfaces, either as a cause or result of osteoarthritis. Subchondral sclerosis and osteophytosis are typically the earliest radiographic osteoarthritis features, which increase in both extent and size as osteoarthritis progresses. These precede the radiographic joint space narrowing that typically occurs at a later stage of the disease.[12-14]
The following are the standard X-ray examinations performed to evaluate knee osteoarthritis:
- Standing anteroposterior view of both knees. It is important that this is done with the patient standing, bearing weight on the joint. It is also important to include both knees for comparison in cases of mild osteoarthritis.
- Lateral view.
- Skyline view of both patellofemoral joints. This is a top-angled view, looking down at the knee caps.
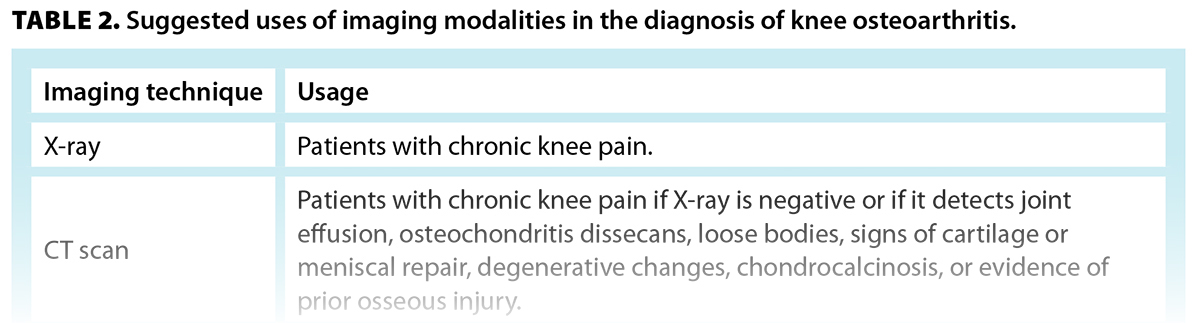
Table 2 summarizes when a certain imaging modality may be useful.[15]
In osteoarthritis, there is no indication for any further imaging. In particular, an MRI scan for patients over the age of 40 is rarely indicated and does not add value for the diagnosis or treatment of osteoarthritis. If proceeding beyond radiography, soft tissues are best imaged using ultrasonography or MRI, and bones are best imaged using CT scan or MRI. The main detectable features of different imaging modalities used in osteoarthritis are summarized in Table 3.
Patient expectations
Educating patients about their diagnosis and the anticipated clinical progression of osteoarthritis has been linked to a better understanding of the origins of their chronic knee pain.[16] Especially during the early stages of osteoarthritis, comprehensive education aims to encourage patients to make lifestyle modifications such as incorporating low-impact exercises into their routine and adopting a balanced diet to facilitate weight loss. These lifestyle changes can significantly improve patients’ quality of life by easing the load on the affected joints, improving mobility, and reducing pain. Exercise in particular strengthens the muscles that support the joints, thereby stabilizing them and improving overall function.
Furthermore, education extends beyond the realm of lifestyle modifications to include information about osteoarthritis as a disease, including causes, effects, progression, and available treatment options. Providing patients with this knowledge empowers them to make informed decisions about their health and actively participate in their own care. This sense of agency can improve their ability to cope with the disease, enhance adherence to treatment plans, and ultimately result in better clinical outcomes. Studies have shown that patients who are more knowledgeable about their condition experience less anxiety and a greater sense of control, which leads to better health outcomes.[17,18]
Summary
Knee osteoarthritis is the most prevalent form of arthritis that affects the knee. In most instances, a detailed patient history and comprehensive physical examination conducted in the family practice setting are sufficient to make a preliminary diagnosis. The diagnosis is most reliably confirmed through characteristic findings on standing knee X-rays, which continue to be the gold standard. Therefore, more advanced imaging techniques should not be routinely requested in patients who present with chronic knee pain, unless the clinical presentation suggests alternative or additional diagnoses that warrant further investigation. Family physicians should focus on early detection, patient education, and lifestyle modifications to manage symptoms and improve patients’ quality of life.
Competing interests
None declared.
This article has been peer reviewed.
 |
| This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. |
References
1. Dillon CF, Rasch EK, Gu Q, Hirsch R. Prevalence of knee osteoarthritis in the United States: Arthritis data from the Third National Health and Nutrition Examination Survey 1991–94. J Rheumatol 2006;33:2271-2279.
2. Barbour KE, Hootman JM, Helmick CG, et al. Meeting physical activity guidelines and the risk of incident knee osteoarthritis: A population-based prospective cohort study. Arthritis Care Res (Hoboken) 2014;66:139-146.
3. Zhang W, Doherty M, Peat G, et al. EULAR evidence based recommendations for the diagnosis of knee osteoarthritis. Ann Rheum Dis 2010;69:483-489.
4. Felson DT, Niu J, Clancy M, et al. Effect of recreational physical activities on the development of knee osteoarthritis in older adults of different weights: The Framingham Study. Arthritis Rheum 2007;57:6-12.
5. Hsu H, Siwiec RM. Knee osteoarthritis. National Library of Medicine, 2022. Accessed 5 January 2023. www.ncbi.nlm.nih.gov/books/NBK507884.
6. Arthritis Alliance of Canada. Osteoarthritis tool. 2017. Accessed 5 January 2023. https://cep.health/media/uploaded/CEP_OATool_2017.pdf.
7. Vitaloni M, Botto-van Bemden A, Sciortino Contreras RM, et al. Global management of patients with knee osteoarthritis begins with quality of life assessment: A systematic review. BMC Musculoskelet Disord 2019;20:493.
8. Sharma L. Osteoarthritis of the knee. N Engl J Med 2021;384:51-59.
9. Carmona R. Knee exam—McMaster MSK examination series [YouTube video]. 2011. Accessed 5 January 2023. www.youtube.com/watch?v=TsN1QoSMZ_Q.
10. National Institute for Health and Care Excellence. Osteoarthritis: Care and management. Clinical guideline [CG177]. Last updated 19 October 2022. Accessed 10 February 2023. www.nice.org.uk/guidance/cg177.
11. Braun HJ, Gold GE. Diagnosis of osteoarthritis: Imaging. Bone 2012;51:278-288.
12. Buckland-Wright JC, Macfarlane DG, Jasani MK, Lynch JA. Quantitative microfocal radiographic assessment of osteoarthritis of the knee from weight bearing tunnel and semiflexed standing views. J Rheumatol 1994;21:1734-1741.
13. Felson DT, Niu J, Guermazi A, et al. Defining radiographic incidence and progression of knee osteoarthritis: Suggested modifications of the Kellgren and Lawrence scale. Ann Rheum Dis 2011;70:1884-1886.
14. Felson D, Niu J, Sack B, et al. Progression of osteoarthritis as a state of inertia. Ann Rheum Dis 2013;72:924-929.
15. Sukerkar PA, Doyle Z. Imaging of osteoarthritis of the knee. Radiol Clin North Am 2022;60:605-616.
16. American Academy of Orthopaedic Surgeons. Management of osteoarthritis of the knee (non-arthroplasty): Evidence-based clinical practice guideline. 2021. Accessed 5 January 2023. www.aaos.org/oak3cpg.
17. Goff AJ, De Oliveira Silva D, Merolli M, et al. Patient education improves pain and function in people with knee osteoarthritis with better effects when combined with exercise therapy: A systematic review. J Physiother 2021;67:177-189.
18. Coudeyre E, Claus D, Ristori J-M. Patient education for osteoarthritis. Presse Med 2010;39:1195-1200.
Mr Darabian completed his undergraduate studies in the Faculty of Arts, University of British Columbia. He is currently a research assistant at the BC Cancer Agency. Dr Badii is a clinical assistant professor in the Division of Rheumatology, Faculty of Medicine, UBC. Dr Wade is a rheumatologist at the Artus Health Centre in Vancouver.
Corresponding author: Mr S. Darabian, saman.darabian@gmail.com.

![TABLE 1. Symptoms of early, moderate, and advanced knee osteoarthritis.[8]](https://bcmj.org/sites/default/files/BCMJ_Vol66_No4_core-diagnosis_web_Table1_post.jpg)
![TABLE 3. Pathologic features of knee osteoarthritis that are detectable by various imaging techniques.[11]](https://bcmj.org/sites/default/files/BCMJ_Vol66_No4_core-diagnosis_web_Table3_post.jpg)