Original Research
Deteriorating wait times for breast cancer patients at a regional hospital in BC, 2013 versus 2023
ABSTRACT
Background: Breast cancer is a common condition, and the number of cases is projected to increase 52% between 2012 and 2030. Care of breast cancer patients occurs along an interdisciplinary continuum involving family physicians, general surgeons, radiologists, pathologists, medical oncologists, radiation oncologists, and allied health workers. There are national benchmarks for wait times between each step from diagnosis to treatment. In this quality improvement project, we sought to measure these wait times at our hospital by comparing results for 2013 and 2023, identifying causes of delays, and proposing solutions to reduce wait times.
Methods: We included all patients who were diagnosed with breast malignancies and referred to the general surgery service at Vernon Jubilee Hospital in 2013 and 2023. Results were analyzed using the two-tailed t test and Fisher exact test for continuous and categorical variables, respectively. A P value less than .05 was considered significant.
Results: The number of patients increased from 69 in 2013 to 113 in 2023. Mean wait times from initial imaging referral to surgery increased from 67 to 114 days (P < .01) during this period. Mean wait times from imaging referral to pathology diagnosis increased from 36 to 71 days (P < .01), due primarily to an increase from 34 to 80 days for symptomatic patients who were referred by their family physician (P < .01); wait times for asymptomatic patients who were identified by the Screening Mammography Program increased from 40 to 58 days (P = .09). Mean wait times from biopsy to final biomarker report (ER/PR/HER2) increased from 25 days to 29 days (P = .25), from surgery to final pathology increased from 11 to 17 days (P < .01), from surgical consultation to surgery increased from 17 to 31 days (P < .01), from referral to medical oncology consultation increased from 14 to 30 days (P < .01), and from referral to radiation oncology consultation increased from 78 to 106 days (P = .025). Most wait times met benchmark wait times in 2013 but failed to meet them in 2023.
Conclusions: Wait times increased at every stage of the care continuum for breast cancer patients between 2013 and 2023 at Vernon Jubilee Hospital. Implementing an interdisciplinary approach to care is necessary to remediate sources of delays at each step. Possible solutions include creating a fast-track pathway for symptomatic patients, performing biomarkers and pathology slide preparation locally, increasing operating room time, and tripling the number of oncologists in the region.
Treating breast cancer is an interdisciplinary endeavor, but delays among the various independently functioning components of the care continuum have contributed to increasing wait times.
Background
 Breast cancer is a common condition among Canadian women, with one in eight diagnosed within their lifetime.[1] Despite stable or decreasing age-standardized incidence, the number of cases in British Columbia is increasing due to population growth and aging. Breast cancer operations in BC increased 28% between 2012 and 2022,[2] and the number of breast cancer cases is projected to increase 52% between 2012 and 2030.[3] Breast cancer care is an interdisciplinary endeavor involving family physicians, general surgeons, radiologists, pathologists, medical oncologists, and radiation oncologists, plus other allied health workers. With the increasing trend in the use of neoadjuvant chemotherapy before surgery in up to 15% of breast cancer cases, multidisciplinary cancer conference discussions are also increasingly required.[4]
Breast cancer is a common condition among Canadian women, with one in eight diagnosed within their lifetime.[1] Despite stable or decreasing age-standardized incidence, the number of cases in British Columbia is increasing due to population growth and aging. Breast cancer operations in BC increased 28% between 2012 and 2022,[2] and the number of breast cancer cases is projected to increase 52% between 2012 and 2030.[3] Breast cancer care is an interdisciplinary endeavor involving family physicians, general surgeons, radiologists, pathologists, medical oncologists, and radiation oncologists, plus other allied health workers. With the increasing trend in the use of neoadjuvant chemotherapy before surgery in up to 15% of breast cancer cases, multidisciplinary cancer conference discussions are also increasingly required.[4]
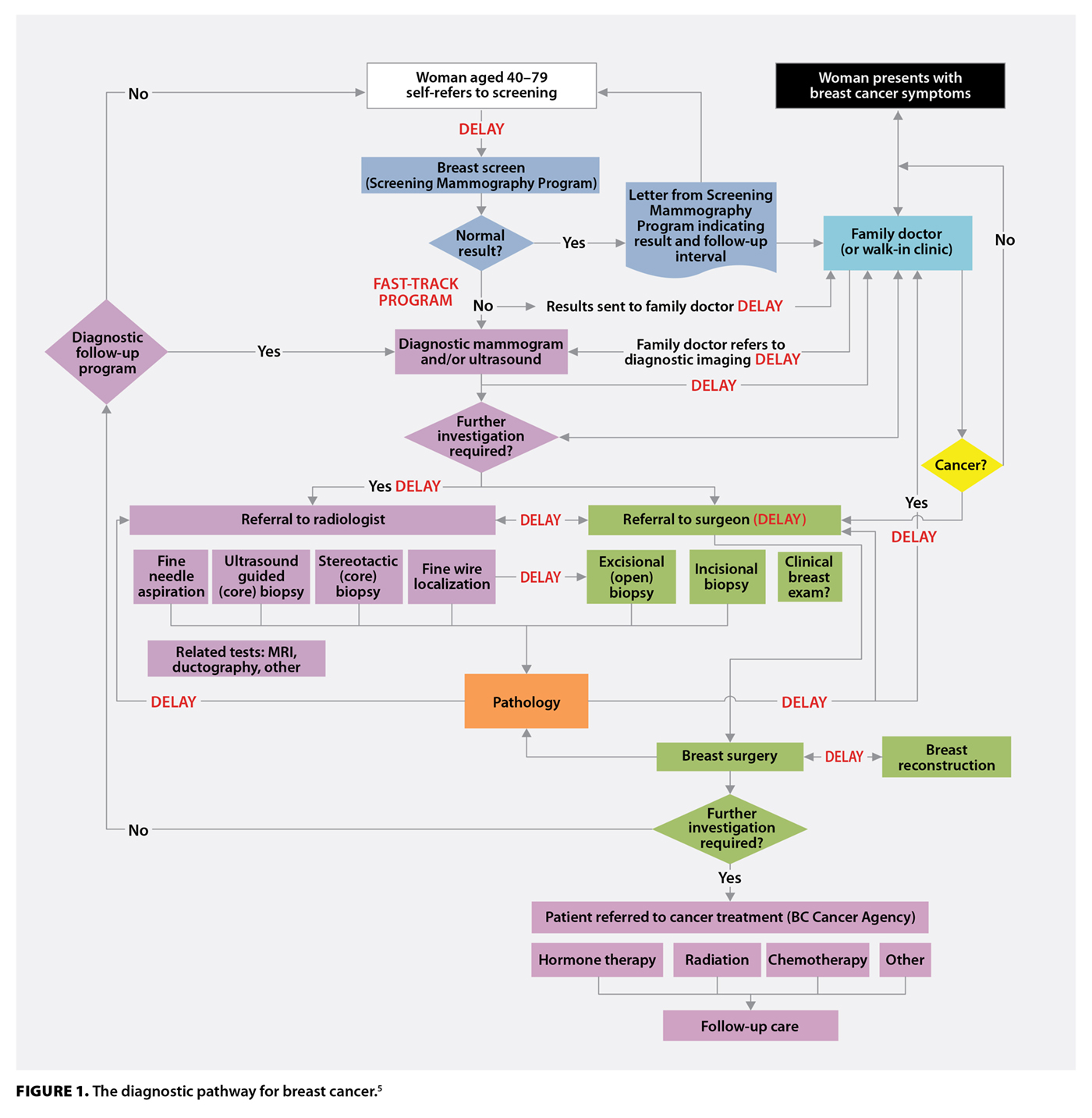
The diagnostic pathway for breast cancer is complicated and fraught with delays, as shown in the Breast Health Action Plan developed in BC in 2010 [Figure 1].[5] The interdisciplinary nature of breast cancer care also leads to silos of care, where groups of physicians focus on their area of specialty with limited coordination with other groups. Without feedback from all physicians involved throughout the entire journey, overall wait times increase.
National benchmarks
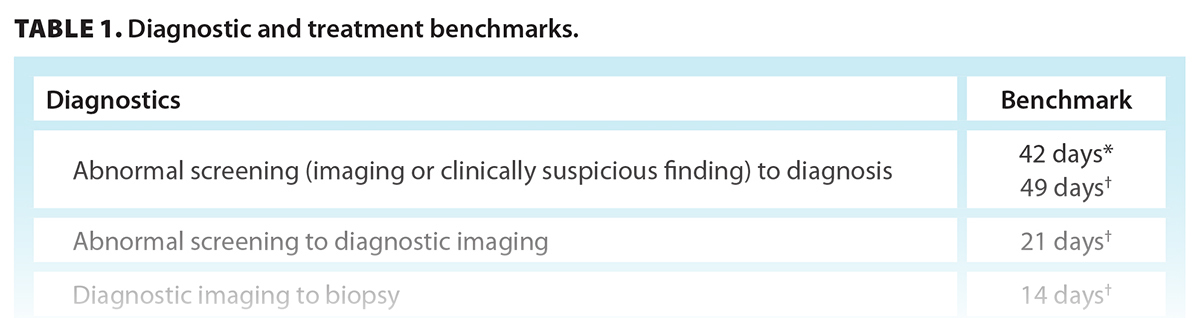
According to the pan-Canadian standards for breast cancer surgery,[6] the benchmark wait time from abnormal breast imaging or clinically suspicious finding to diagnosis is 42 days; core biopsy pathology should be reported within 7 days; biomarker results should be reported “in a timely manner”; surgical consultation should occur within 14 days of referral; final pathology should be reported within 14 days; surgery, chemotherapy, and/or radiation therapy should be initiated within 28 days of oncology consultation; and adjuvant chemotherapy should be initiated within 84 days of surgery. Twenty-one days from abnormal screen or symptomatic presentation to diagnostic result has also been proposed.[7]
According to Health Canada’s Quality Determinants of Organized Breast Cancer Screening Programs in Canada, the time from abnormal screening to first assessment should be 21 days, the time from first assessment to diagnosis should be 28 days, and total duration from abnormal screening to diagnosis should be 49 days.[8] The benchmark for referral to radiation oncology consultation is 28 days.[9] According to the head of BC Cancer,[10] the benchmarks for referral to medical oncology consultation and for radiation oncology consultation to radiotherapy initiation are also 28 days. Therefore, the wait time from referral to chemotherapy or radiotherapy should be 56 days (28 + 28 days). These are the benchmark standards we used in our comparisons [Table 1].
Objective
Our objective was to quantify wait times across the continuum of interdisciplinary breast cancer care, identify causes of delays, and propose solutions to shorten the overall time from diagnosis to treatment of breast cancer at our hospital.
Methods
This quality improvement project was screened for ethics using the ARECCI tool[11] and deemed low-risk; therefore, it did not require a formal ethics review.
We included all patients who were diagnosed with invasive breast carcinoma, ductal carcinoma in situ, or phyllodes tumors of the breast and referred to the general surgery service at Vernon Jubilee Hospital (VJH), a 196-bed regional hospital in the Regional District of North Okanagan. We limited the comparison to the calendar years of 2013 and 2023. Cases of benign breast lesions were excluded.
Using a combination of family physician or surgeon office chart review and review of hospital and BC Cancer electronic records, the following dates were recorded: referral for breast imaging, screening mammogram, diagnostic mammogram, focused ultrasonography, breast biopsy, reporting of biopsy pathology, reporting of biomarkers, referral to general surgeon, general surgeon consultation, surgery date, referral to cancer agency, medical oncology consultation, radiation oncology consultation, chemotherapy initiation, and radiotherapy initiation. We also noted whether patients required neoadjuvant chemotherapy, surgical procedure, and pathology diagnosis.
We used the two-tailed t test to compare continuous variables and the Fisher exact test to compare categorical variables using an online calculator.[12] Confidence intervals were calculated using Microsoft Excel. A P value less than .05 was considered significant.
Results
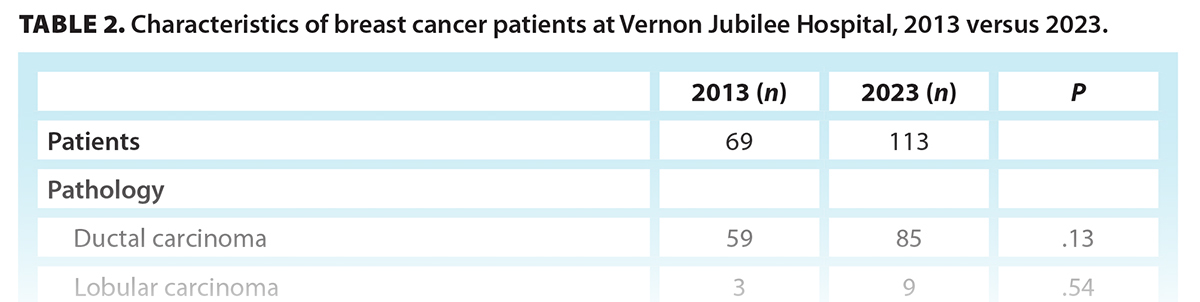
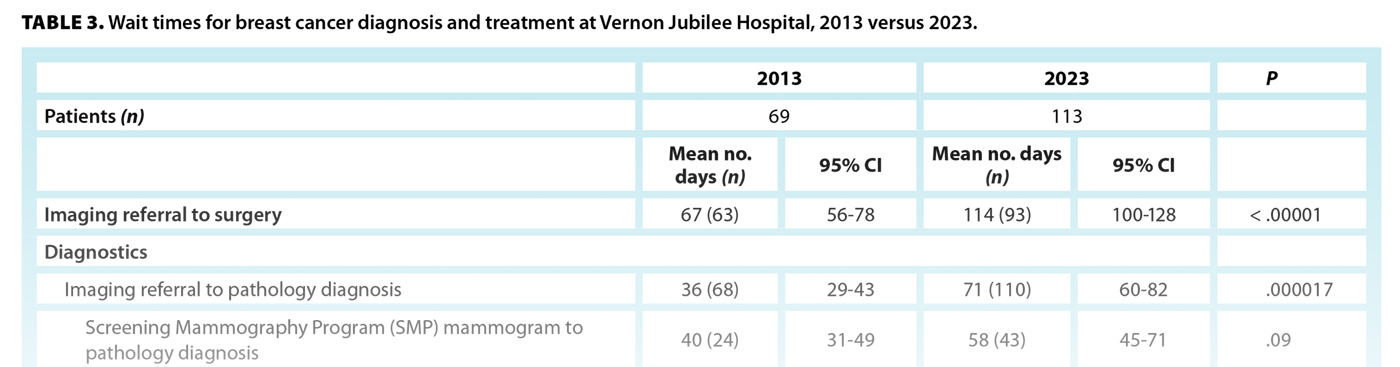
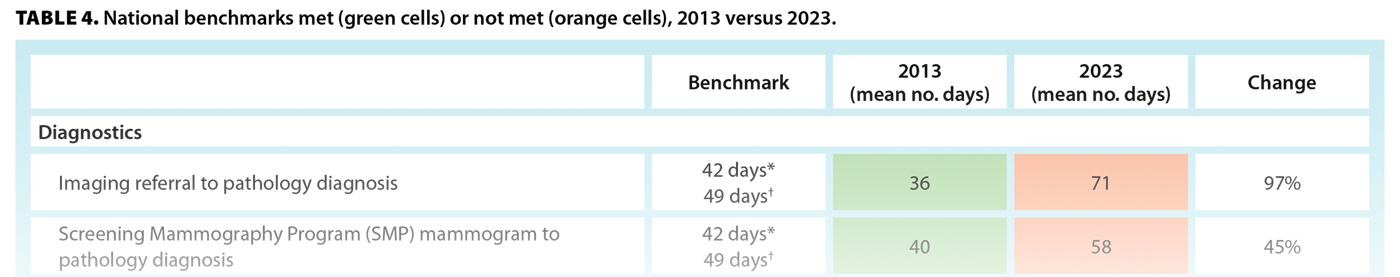
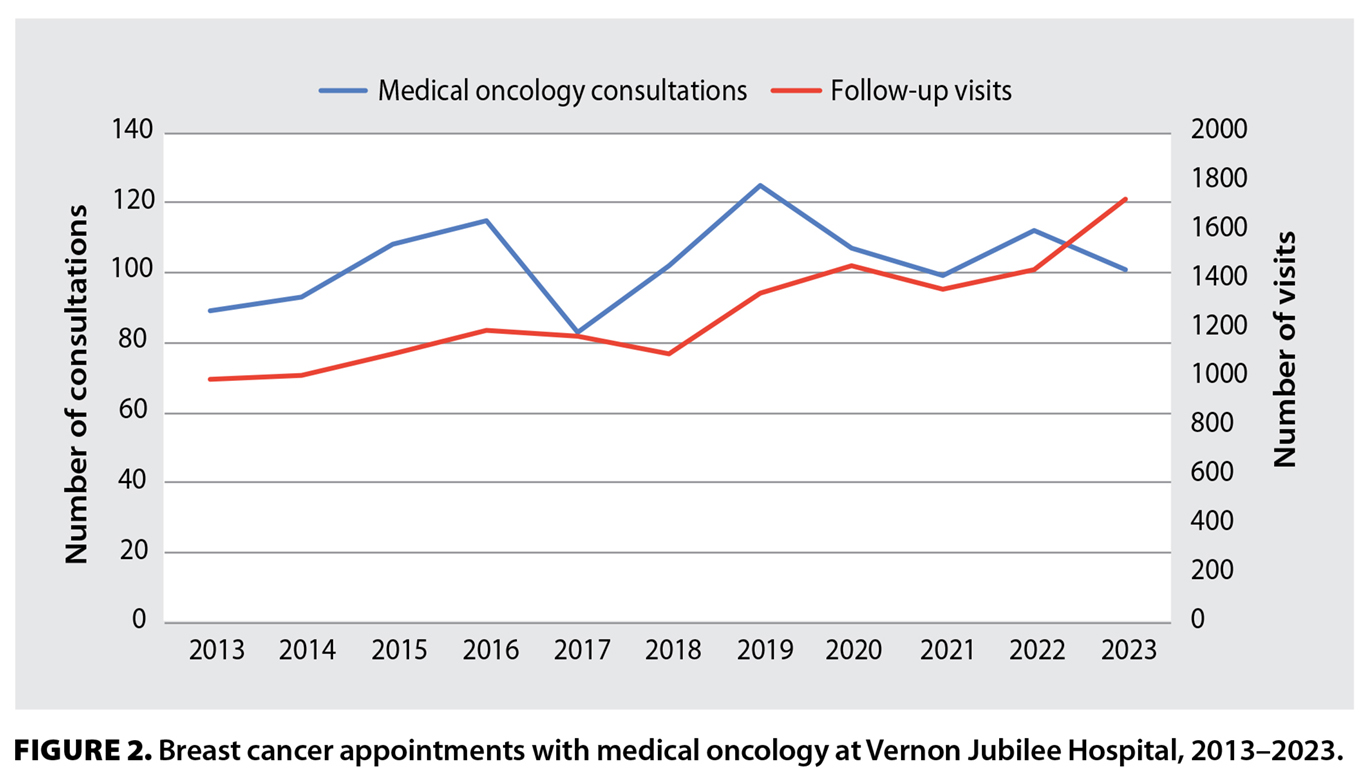 The number of breast cancer cases referred to the general surgery group at VJH increased from 69 in 2013 to 113 in 2023 (64%). Figure 2 shows the number of breast cancer appointments with medical oncology at VJH during this period. Table 2 shows patient characteristics in 2013 versus 2023. Table 3 summarizes the various wait times. The mean overall wait from initial imaging referral to surgery increased from 67 days in 2013 to 114 days in 2023 (P < .01). Table 4 shows the benchmark wait times that were met and not met in 2013 versus 2023.[6,8-10]
The number of breast cancer cases referred to the general surgery group at VJH increased from 69 in 2013 to 113 in 2023 (64%). Figure 2 shows the number of breast cancer appointments with medical oncology at VJH during this period. Table 2 shows patient characteristics in 2013 versus 2023. Table 3 summarizes the various wait times. The mean overall wait from initial imaging referral to surgery increased from 67 days in 2013 to 114 days in 2023 (P < .01). Table 4 shows the benchmark wait times that were met and not met in 2013 versus 2023.[6,8-10]
Diagnostics
There were significant increases in diagnostic wait times from 2013 to 2023 [Table 4]. Many wait times that met benchmarks in 2013 no longer did so in 2023. In particular, patients who presented to their family physician with symptoms such as a palpable mass (family physician referral) experienced larger increases in wait times than patients without symptoms who were identified through the Screening Mammography Program.
The wait time from biopsy to final biomarker reporting did not increase significantly from 2013 to 2023, but it was already 25 days in 2013. In many cases, the final biomarker reporting was after the surgery date. Table 2 shows that in both years, the biomarkers for several patients who were either triple-negative or HER2-positive and did not receive neoadjuvant chemotherapy were reported in a non-useful time frame (either less than 7 days before the surgery date or after the surgery date).
Wait-one time
Wait-one time is defined as the time from primary care referral to surgical consultation. It increased from 10 to 14 days from 2013 to 2023 but was not a significant increase [Table 3], and it met the benchmark of 14 days in both time periods [Table 4].
Wait-two time
Wait-two time is the time from surgical consultation to operation. It increased significantly from 17 to 31 days from 2013 to 2023 [Table 3]. The wait time met the benchmark in 2013 but failed to meet it in 2023 [Table 4].
Oncology referral and treatment
The wait time for referral to medical oncology consultation increased significantly from 14 to 30 days from 2013 to 2023 [Table 3], and in 2023, it failed to meet the 28-day benchmark [Table 4]. The wait time for referral to chemotherapy initiation did not increase significantly [Table 3] and met the benchmark in both periods [Table 4]. The wait from surgery to adjuvant chemotherapy did not increase significantly [Table 3] and met the benchmark in both periods [Table 4]. The wait time for medical oncology consultation to chemotherapy initiation decreased slightly but not significantly from 2013 to 2023 [Table 3] and met the benchmark in both periods [Table 4].
For patients who required neoadjuvant chemotherapy, the wait time from referral to the cancer agency for chemotherapy initiation increased from 18 days (n = 3, 95% CI 8-28) to 27 days (n = 12, 95% CI 22-32) but was not significant (P = .12) and met the 56-day benchmark in both periods.
The wait time for referral to radiation oncology consultation increased significantly from 2013 to 2023 but not for referral to radiotherapy initiation [Table 3]; however, the wait times for both failed to meet the benchmark in both years [Table 4]. The wait time from radiation oncology consultation to radiotherapy initiation decreased from 2013 to 2023 but not significantly [Table 3] and failed to meet the benchmark only in 2013 [Table 4].
Discussion
Wait times for both diagnosis and treatment of breast cancer at VJH increased significantly from 2013 to 2023, and several benchmarks that were met in 2013 were not met in 2023. The overall wait time from abnormal imaging to surgery increased from 67 days in 2013 to 114 days in 2023 and did not compare favorably to a median wait time of 52 days in Ontario for 2003 to 2011[13] (Ontario data are not available for 2013 or 2023).
The 64% increase in breast cancer referrals to general surgery in our study was higher than the 13% increase in new breast cancer medical oncology consultations from 2013 to 2023. It was also greater than the 28% increase in breast cancer operations conducted provincially between 2012 and 2022.[2] This could be explained by the fact that some referrals from outside the Regional District of North Okanagan were diverted to other centres by the local medical oncology service due to a shortage of medical oncologists at VJH in 2023, while surgeons continued to accept out-of-region referrals. Additionally, in the North Okanagan and Columbia–Shuswap Regional Districts, the population aged 65 years or older increased 43% between 2013 and 2023.[14]
Delays in imaging—A prominent contributor
Abnormalities are detected in 9.1% of screening mammograms, and 6.1% of those are diagnosed as cancer.[15] Shorter wait times for diagnosis have been achieved by coordinating radiologic and clinical care[16]—for example, by adopting a policy of completing diagnostic workups without requiring new requisitions or keeping dedicated rapid-access appointments for breast biopsy within a short period, such as less than 1 week. This might improve the rate of same- or next-day biopsies after abnormal diagnostic imaging, which declined significantly from 57% in 2013 to 16% in 2023 in our study. A possible factor in the decline in same-day biopsies was a shortage of radiologists at our hospital in 2023, which was not an issue in 2013. Without radiologists, image-guided biopsies cannot be performed; this applies not only to breast lesions but also to other organs that require tissue diagnosis. Improving radiologist human resources should be a high priority in our health region.
Establishing a breast health clinic such as the one based in Kamloops[17] and employing a nurse navigator[18] can also reduce wait times, but this is dependent on additional funding. Strategies to reduce wait times for diagnostic imaging without obtaining additional funding could include a fast-track pathway for high-suspicion symptomatic patients.
The Screening Mammography Program has dedicated resources for monitoring wait times and other outcomes. There is no equivalent monitoring system for symptomatic patients who are referred by their family physician, which has likely led to the unintended discrepancy in wait times between the two groups in our study. There should be an annual audit of wait times for symptomatic patients to ensure outcomes are equivalent to those of Screening Mammography Program patients.
Biomarkers logistics—A major problem
Biomarkers, estrogen/progesterone, and HER2 receptors are crucial factors that impact clinical decision making. Delays in reporting lead to delays in surgery or oncology consultation. Sixteen percent of our patients had triple-negative or HER2-positive disease. Ideally, these cases should be discussed at multidisciplinary conferences and locally attended by general surgery, radiology, pathology, and oncology, and those with larger tumors or positive nodes should be considered for neoadjuvant chemotherapy before surgery.[4] However, less than half the cases of potentially eligible patients in our study were discussed at multidisciplinary conferences, and the biomarkers of half those patients were reported either within 7 days of the operating room date or even after the surgery was completed. We believe biomarkers should be reported within 7 days of the biopsy, but this was not possible due to logistical issues. The testing was done only in Vancouver and required samples to be transported between centres. If immunohistochemistry interpreted the HER2 receptor as “equivocal,” then in situ hybridization testing led to further delays. The results were reported on one system at BC Cancer, but they did not seamlessly transfer to the local health authority system. Therefore, workarounds were required, which were not consistent and led to triple-negative or HER2-positive status sometimes being discovered only after the surgery had been performed. It should be noted that although proportionally fewer patients underwent surgery in 2023 without having biomarker results available compared with those in 2013, this was not due to improved biomarker reporting times. Rather, in many cases, surgery was delayed because the consensus at the multidisciplinary conference was that neoadjuvant chemotherapy might be necessary and dependent on the results. To reduce the turnaround time to acceptable levels, both immunohistochemistry and in situ hybridization testing of biomarkers should be performed within the region, either in Kelowna or locally in Vernon, and not in Vancouver. In addition, the attending surgeon should be identified through a centralized referral pathway so they can be copied on any biomarker result addenda to the original biopsy.
Lack of local pathology processing
There was a significant increase in the time from surgery to the final pathology results. This is also crucial information that impacts and delays adjuvant treatment. Processing of pathology specimens (embedding, cutting, and slide generation) is currently performed in Kelowna, though previously it was done locally in Vernon. This service should be re-established to reduce wait times and help expedite oncology treatments.
Operating room access below the provincial average
Delays from diagnosis to surgery can lead to increased mortality.[19] Though the wait time from referral to surgical consultation in our study did not increase significantly and remained within benchmarks in both years, shorter wait times to surgery have been achieved with centralization of surgical referrals.[20] This should be implemented at VJH to equalize surgical wait times.
The 2021 median wait time for breast cancer surgery in Canada was 18 days.[9] The 17-day mean and 15-day median surgical wait times in 2013 in our study compared favorably with this, but the 31-day mean and 28-day median wait times in 2023 did not. The 82% increase in mean wait time from general surgery consultation to operation in our hospital could be explained by a relative shortage of operating room access compared with the rest of BC. While breast cancer cases increased 64% from 2013 to 2023 in our study, operating room time for the general surgery service increased only 10%, from 20 to 22 operating room days per month. The mean number of operating room days per surgeon per month in our study was 4.0 (20 days/5 surgeons) in 2013 and 3.1 (22 days/7 surgeons) in 2023; the mean in BC was 4.2 in 2022.[2] Increasing operating room access to match the provincial average would require an additional 7.5 operating room days per month, which would help reduce wait times.
Extreme oncology human resource challenges
Once patients saw either a medical or radiation oncologist, their treatment initiation was very prompt and was even significantly reduced for radiotherapy in 2023 compared with 2013. However, the wait time to see a medical oncologist more than doubled from 2013 to 2023. In some instances, the delays were due to biomarker reporting times or those for Oncotype DX results, genetic tests on the breast tumor that are performed in California; however, this was not the major factor. Most delays to see a medical oncologist were due to human resource shortages at our local BC Cancer clinic. In 2023, many patients were diverted to other centres in the region, which had resource challenges of their own.
Waiting more than 84 days for radiotherapy has been associated with poorer outcomes.[21] In our study, the wait time for radiotherapy was already unacceptably long in 2013 (114 days), greater than the 56-day benchmark, but then increased even more to 143 days in 2023 (25%). This also points to a major shortage in human resources; the wait times will continue to worsen unless this shortage is addressed. We estimate that three times the number of current medical and radiation oncologists in the region are needed to handle the current demand.
Study limitations
This project was limited to key dates along the breast cancer care continuum and did not delve into individual reasons for delays, such as those due to patient reluctance toward investigation or treatment. It also shows wait times only at VJH, though we believe the results are generalizable to other facilities throughout the province because many of the issues we identified are systemic and not limited to VJH. Another important limiting factor was the severe shortage of primary care physicians and the associated impact on patients without a family doctor who had limited access to the Screening Mammography Program or investigation of a new breast lump. Additionally, the wait time from self-referral to screening mammography was unknown, because these data were not available.
Conclusions
Treating breast cancer is an interdisciplinary endeavor, but this is a source of weakness, because delays among the various independently functioning components along the care continuum contribute to overall increasing wait times. Our study showed that the wait times from referral to surgery increased from 67 days in 2013 to 114 days in 2023 (70%), the wait from referral to radiotherapy increased from 114 to 143 days in the same period, and extremely slow biomarker reporting compounded delays. An interdisciplinary approach to each component of the delay is necessary to improve patient outcomes. The Box lists our recommendations for improving wait times for each component along the continuum of care for breast cancer patients at VJH.
Funding
This project was funded by the Vernon Jubilee Hospital Physician Society, a branch of the Specialist Services Committee’s Facility Engagement Initiative.
Competing interests
None declared.
BOX. Recommendations for improving wait times for breast cancer diagnosis and treatment at Vernon Jubilee Hospital.
Diagnostics:
- Complete imaging workup without requiring new requisitions.
- Keep dedicated rapid-access appointments for image-guided biopsy within 1 week.
- Establish a fast-track pathway for high-suspicion symptomatic patients.
- Perform annual audits of imaging wait times for symptomatic patients to ensure outcomes are equivalent to those for Screening Mammography Program patients.
- Perform biomarker testing within the region.
- Identify attending surgeons early through a centralized referral pathway so they can be copied on biomarker results.
- Re-establish pathology slide processing locally.
Wait-one time:
- Establish centralized referral for surgical consultation.
Wait-two time:
- Increase operating room time for the Vernon Jubilee Hospital general surgery service by 7.5 days per month to meet the provincial average of 4.2 operating room days per surgeon per month.
Oncology:
- Triple the number of medical and radiation oncologists in the region.
This article has been peer reviewed.
 |
| This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. |
References
1. Canadian Cancer Statistics Advisory Committee, Canadian Cancer Society, Statistics Canada, Public Health Agency of Canada. Canadian cancer statistics 2023. Toronto, ON: Canadian Cancer Society, 2023. Accessed 11 February 2024. https://cancer.ca/Canadian-Cancer-Statistics-2023-EN.
2. Hwang H, Samarasinghe N, D’Souza K, et al. Chasing a moving train: The general surgery workforce versus population growth in British Columbia, 2012–2022. BCMJ 2024;66:46-50.
3. Woods RR, Coppes MJ, Coldman AJ. Cancer incidence in British Columbia expected to grow by 57% from 2012 to 2030. BCMJ 2015;57:190-196.
4. Warburton R, Chui CG, Roberts A, et al. Current surgical management of breast cancer. BCMJ 2018;60:92-98.
5. Provincial Health Services Authority. Breast health action plan. 2010. Accessed 18 February 2024. www.phsa.ca/professional-resources-site/PublishingImages/health-professionals/professional-resources/provincial-breast-health-strategy-2/Breast_Health_Action_Plan.pdf.
6. Canadian Partnership Against Cancer. Pan-Canadian standards: Breast cancer surgery. 2019. Accessed 11 February 2024. https://s22457.pcdn.co/wp-content/uploads/2019/05/Breast-Cancer-Surgery-Standards-EN-April-2019.pdf.
7. Wilson C, Kuusk U, Dingee C, et al. Coordination of radiological and clinical care for breast cancer diagnosis in BC. BCMJ 2018;60:33-39.
8. Health Canada. Quality determinants of organized breast cancer screening programs in Canada. 2003. Accessed 17 February 2024. https://publications.gc.ca/collections/Collection/H39-407-2003E.pdf.
9. Canadian Institute for Health Information. Wait times for priority procedures in Canada, 2022. 2022. Accessed 11 February 2024. www.cihi.ca/en/wait-times-for-priority-procedures-in-canada-2022.
10. DeRosa K. Province’s cash injection for BC. Cancer aimed at trimming long waits for care. Vancouver Sun. 27 February 2023. Accessed 22 February 2024. https://vancouversun.com/news/local-news/provinces-cash-injection-for-b-c-cancer-aimed-at-trimming-long-waits-for-care.
11. Alberta Innovates. ARECCI Ethics Screening Tool. Accessed 1 January 2024. https://arecci.albertainnovates.ca.
12. Social Science Statistics. Statistics calculators. Accessed 11 February 2024. www.socscistatistics.com/tests.
13. Cordeiro E, Dixon M, Coburn N, Holloway CMB. A patient-centered approach to wait times in the surgical management of breast cancer in the province of Ontario. Ann Surg Oncol 2015;22:2509-2516.
14. BC Stats. Population estimates and projections for British Columbia. Accessed 24 February 2024. https://bcstats.shinyapps.io/popApp/.
15. Mar C, Sam J, Wilson C. Breast cancer screening in British Columbia: A guide to discussion with patients. BCMJ 2018;60:20-26.
16. McKevitt EC, Dingee CK, Warburton R, et al. Coordination of radiologic and clinical care reduces the wait time to breast cancer diagnosis. Curr Oncol 2017;24:e388-e393.
17. Ewart E, Barton A, Chen L, et al. Assurance of timely access to breast cancer diagnosis and treatment by a regional breast health clinic serving both urban and rural-remote communities. Curr Oncol 2023;30:1232-1242.
18. Baliski C, McGahan CE, Liberto CM, et al. Influence of nurse navigation on wait times for breast cancer care in a Canadian regional cancer center. Am J Surg 2014;207:686-691.
19. Hanna TP, King WD, Thibodeau S, et al. Mortality due to cancer treatment delay: Systematic review and meta-analysis. BMJ 2020;371:m4087.
20. Cha J, McKevitt E, Pao J-S, et al. Access to surgery following centralization of breast cancer surgical consultations. Am J Surg 2020;219:831-835.
21. Raphael MJ, Saskin R, Singh S. Association between waiting time for radiotherapy after surgery for early-stage breast cancer and survival outcomes in Ontario: A population-based outcomes study. Curr Oncol 2020;27:e216-e221.
Dr Hwang is a general surgeon at Vernon Jubilee Hospital (VJH) and head of the VJH Division of General Surgery. Dr Parker is a general surgeon at VJH. Dr Horkoff is a general surgeon at VJH and deputy head of the VJH Division of General Surgery. Drs Humphreys and Hardy are medical oncologists at VJH. Dr McClellan is a family physician at VJH and head of the VJH Department of Family Medicine. Dr Brierley is a general pathologist at VJH and head of the VJH Department of Pathology. Dr Brosseau is a radiologist at VJH. Mrs Rempel is a clinical operations manager at VJH.