Canada’s largest purpose-built public day-care surgery centre: A retrospective audit of patients requiring transfer to an inpatient hospital
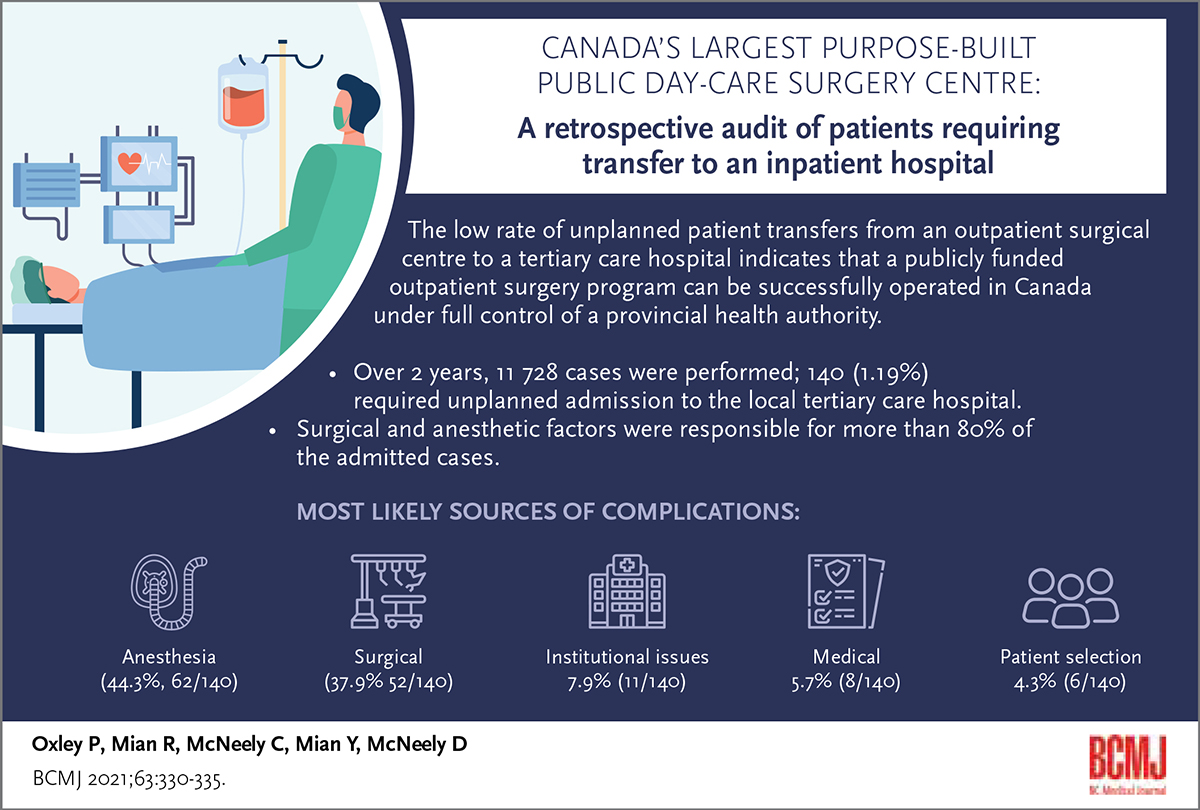
ABSTRACT: Rapid growth in regional population puts an incredible strain on health care resources. Our health authority attempted to reduce this burden by building a large, standalone outpatient care and surgery centre. To determine the success of this surgical program, we undertook a review of a 2-year period for all cases performed in the main operating room with an anesthetist present to determine successful discharge rates for these day-care cases. We also set out to determine factors responsible for unsuccessful discharge cases requiring admission to the local tertiary care hospital. Over 2 years, 11 728 cases were performed, with 140 (1.19%) requiring unplanned admission. Surgical and anesthetic factors were responsible for more than 80% (115/140) of these admitted cases. A large standalone centre can successfully provide high-volume surgical care with a very low unplanned admission rate. These programs can greatly assist in offloading regional hospitals and reducing surgical admissions.
The low rate of unplanned patient transfers from an outpatient surgical centre to a tertiary care hospital indicates that a publicly funded outpatient surgery program can be successfully operated in Canada under full control of a provincial health authority.
Background
The Fraser Health Authority is the largest and fastest growing health region in BC.[1] This rapid growth has put considerable pressure on local hospitals to deliver outpatient clinic, diagnostic, and surgery services. In response, the Ministry of Health designed and built a stand-alone, dedicated outpatient and surgery facility—the Jim Pattison Outpatient Care and Surgery Centre (JPOCSC). One of the main goals of the facility is to provide ambulatory surgical services to help alleviate demand on hospital operating rooms and expand overall surgical capacity in Fraser Health. The centre received significant public funding, but donor funding from the Surrey Hospitals Foundation, private donors, and ultimately Mr Jim Pattison accounted for a portion of the equipment costs.
Many studies have examined the key attributes of successful day-care surgery programs[2-4] and have helped define patient health cutoffs for BMI, age, American Society of Anesthesia (ASA) level, and other variables. Enhanced recovery after surgery initiatives have greatly improved outpatient success,[5-7] and most surgical specialties have tried to identify those procedures that can be safely performed in a day-care surgery setting.[8-14] Most larger studies[2,15] have focused on one surgical specialty. Recent anesthesia focus has been on the effect of obstructive sleep apnea on day-care surgery success rates.[16] While studies have been conducted outside Canada,[17-19] there have been no recent reviews of large day-care surgery centres in this country. In addition, most stand-alone surgical facilities in Canada are privately built and operated, which can lead to patient selection bias.
In any ambulatory surgery centre, programming to prevent and reduce complications that require patient transfer to a higher level of care or hospital admission is essential. Once those factors have been identified, it is also important to compare local results with national or international averages. JPOCSC submits data to the National Surgical Quality Improvement Program (NSQIP) database and uses it as a source of quality control.
We set out to identify unplanned transfers from JPOCSC to the local tertiary care hospital, identify factors that led to those events, allocate those factors to specific aspects of the patient care pathway, and compare our results to NSQIP baselines. We also set out to demonstrate the viability of large, stand-alone, publicly run day-care surgery centres within the Canadian health care system.
Methods
All patients who underwent surgical procedures at JPOCSC from 1 January 2016 to 31 December 2017, including those who had a procedure with general anesthesia in a full-service operating theatre, were included in our study. Procedures performed in minor theatres that did not require general anesthesia were not included.
All patients who required transfer to the local tertiary care centre prior to discharge were identified, and their charts were reviewed to determine the most likely reason for transfer. We then categorized each transfer case by the most likely source of complication, as follows: surgical, medical, anesthesia, patient selection, and process (institutional). In cases where more than one factor was identified, only the most significant was categorized, as determined by a group consisting of a nurse, anesthetist, and surgeon. For example, if a patient had significant postoperative pain and required cardiac monitoring, the cardiac issue was determined to be the more significant reason for transfer. All transfer cases involved patients who could not be discharged home for any reason; they did not include patients who were discharged and readmitted at a later date.
We also reviewed the readmission rate within 1 week of discharge to capture any outliers. These data were further subdivided by surgical subspecialty.
Finally, NSQIP data for the same time period[20] as our study were used as a benchmark for comparing our results to the national average.
Results
During the 2-year study period, 11 728 procedures were conducted at the JPOCSC. Table 1 lists the most commonly performed procedures according to surgical discipline. In total, 140 cases required transfer to the local tertiary care hospital.
Over the 2-year period, the discharge rate was 98.81%, and the transfer rate was 1.19%. Annual transfer rates were similar: 1.24% in the first year; 1.16% in the second year.
The average number of ambulatory surgeries performed per month at JPOCSC over the 2-year period was 488 (range 398–627) [Figure 1]. The average number of transfers per month was 5.8 (range 2–10) [Figure 2]. The transfer rate per month [Figure 3] refers to the number of transfers as a percentage of total case number. It ranged from 0.35% to 2.22%, with the average rate for all dates of 1.19%.
The categories most commonly associated with transfers over the 2-year period were anesthesia (44.3% [62/140]) and surgical (37.9% [53/140]) [Table 2]. Institutional factors were responsible for 7.9% (11/140) of all transfers, while medical and patient selection factors led to 5.7% (8/140) and 4.3% (6/140) of all transfers, respectively.
We also examined the total number of transfers per surgical discipline [Table 3]. In both years of the study, most transfers were associated with general surgery and plastic surgery. Retinal surgery was the only category not associated with transfers in either year.
Most unplanned readmissions occurred in the first 48 hours following discharge after surgery. The overall readmission rate was 1.81% for all surgical disciplines over the 2 years [Table 4]. The highest readmission rates were associated with urology, general surgery, orthopaedics, and ear, nose, and throat.
Discussion
Surgery continues to evolve to try to create less invasive, safer, and more expedient procedures. In addition, increasing numbers of procedures that once required lengthy inpatient stays have been switched to day-care surgery procedures.[7,8,11-15] This has resulted in benefits such as reduced nosocomial infections and reduced costs.
There are many private surgical facilities in Canada that have been built predominantly to provide noninsured services, such as cosmetic surgery, or surgery covered outside the standard provincial health care systems. The Canadian surgical system has been largely hospital based, though increasing numbers of surgeries are being contracted out to private centres to help alleviate hospital surgical volumes.[21] There is no doubt that these centres can provide an excellent same-day discharge rate.[2] Due to provincial College of Physician restrictions, the cutoffs for patient variables, such as BMI, that allow for outpatient surgery are often stricter than those that a hospital can use. This limits the number of patients who can receive surgery at an outpatient facility.
Our review included all procedures performed in a full-service operating room with general anesthesia and cases, such as spinal cases or regional cases, where anesthesia was present; therefore, cases such as routine gastroscopy, colonoscopy, vasectomy, minor skin surgery, and minor hand surgery were not included. These procedures, performed with local anesthetic with or without quick reversal sedation, are widely accepted outpatient procedures. In addition, other procedures commonly performed on an outpatient basis, such as cataract surgery, are not performed at the JPOCSC. All patients were ASA 1 or 2 except vascular-access patients and patients with pacemakers who could be ASA 3 as well. A BMI limit of 45 was used, and patients with a significant history of obstructive sleep apnea or anesthetic complications are not permitted to have surgery at JPOCSC. Because operating room access at both JPOCSC and the tertiary care hospital is tied to the same allocation algorithm, many patients who would qualify for surgery at JPOCSC received their care at the tertiary care hospital to expedite access. Therefore, most day-care surgeries, regardless of location, received care from the same surgeon and anesthetic team.
When JPOCSC was created, the regional hospital’s criteria for day-care surgery were adopted because JPOCSC’s size and scope made it possible to treat more complex patients, and its close tie to the hospital made transfers easier, without refusal. The overall intent was to not limit the cases that would be conducted on an outpatient basis at one facility versus the other.
There can be a significant difference in the same-day discharge rate of a day-care surgical centre versus that of a hospital. Our team identified a significantly higher same-day discharge rate for an outpatient centre compared to that of a hospital when all other variables were controlled.[12] We also found an institutional bias in admitting: the rate was almost 9 times higher at the hospital than at the day-care surgical centre, due largely to the ease of admitting. The discharge rate at the local tertiary care hospital matched that reported by a different group in another province[22] for the same procedures, which further shows institutional bias when admission is a much simpler process. Therefore, a stand-alone outpatient centre has a greater chance of optimizing same-day discharge on a routine basis.
JPOCSC was opened to provide ambulatory day-care surgery to reduce volumes in the main hospital operating rooms and increase overall surgical capacity in Fraser Health. Since the surgeries performed can be relatively complex for day-care surgery, often beyond the scope of most free-standing ambulatory centres, it is important to continuously monitor the transfer rate from JPOCSC to a higher level of care and to compare the rate to that of similar institutions.
We determined that for the 11 728 surgeries performed over the 2-year period in this study, the unplanned transfer rate was 1.19%. This is similar to results in a report produced by multiple ambulatory surgery centres in the United States in 2017.[20] That study included 1499 ambulatory centres and 1 749 059 surgeries. The rate of hospital transfer and admission was 1.01%. Our transfer rate was within the middle 50th percentile for all centres. We used the NSQIP data because ambulatory centres are much more common in the United States; therefore, a larger database of comparative result was available. Our transfer rate also declined from 1.24% to 1.16% between the first and second years of study, even though more surgeries were performed in the second year.
The low number of transfers in our study and others suggests that ambulatory centres do not need to be immediately adjacent to a larger hospital. This can allow health authorities and governments to choose locations closer to new centres of population growth to improve resource distribution.
Paramount to determining the viability of successful outpatient discharge is the review of unplanned readmission within a specific period following surgery. Our overall rate of readmission within the first week following surgery was 1.81% for all surgical disciplines. This rate was within the NSQIP mid-50th percentile for similar centres over the same time period.[20] For all cases, readmission was due to surgical complications such as hematoma or surgical site infection. In our review of readmissions, combined general surgery and plastic surgery breast reconstruction cases were placed in the plastic surgery group. This readmission rate is similar to the rate recorded at the regional hospital for similar cases, and is within the NSQIP average range.
In this study, the cause that was most likely responsible for patient transfer was examined. All reasons for transfer were then grouped into surgical, medical, anesthetic, institutional, and patient selection categories. The categories naturally had some crossover between groups. It is very difficult to isolate pain into either the anesthetic or surgical categories. This issue has been brought before both disciplines at JPOCSC for review. For simplification, we included postoperative pain under anesthesia.
Each case transferred from JPOCSC is presented to each member of the patient care pathway and is reviewed at divisional morbidity and mortality rounds, as are readmissions. This has proven beneficial to obtaining input from different parts of the care pathway. Other studies have shown that this type of review is essential to improving patient care outcomes.[19,23-25]
Conclusions
The JPOCSC and Surgery Centre’s unplanned transfer and admission rate to the tertiary care hospital was well within the average for similar centres throughout the United States. The very high success rate for same-day discharge eclipsed that of case-controlled patients who had the same surgery at a regional tertiary care hospital. The lack of overnight stay capability at JPOCSC encourages adherence to the patient care pathway, and our low readmission rate postdischarge further indicates the successful same-day discharge of these patients.
In our public health care system, it is crucial to maximize resource use and patient access to services. Unplanned overnight admissions following surgery unnecessarily tie up inpatient beds and add further expense to the already taxed public system.
A publicly funded outpatient surgery program can be successfully operated in Canada under full control of a provincial health authority.
Competing interests
Three of the authors (Oxley P., Mian R., and McNeely D.) have privileges at the Jim Pattison Outpatient Clinic and Surgery Centre. Two of the authors (Oxley P. and Mian R.) are also part owners of a private clinic. No outside funding was received for this project.
This article has been peer reviewed.
References
1. Fraser Health Careers. Accessed 14 July 2020. https://careers.fraserhealth.ca/work-here/.
2. Rohrich RJ, Mendez BM, Afrooz PN. An update on the safety and efficacy of outpatient plastic surgery: A review of 26,032 consecutive cases. Plast Reconstr Surg 2018;141:902-908.
3. Evans GRD, Scholz T, Brandt K. Outpatient surgery. Plast Reconstr Surg 2015;136:89e-95e.
4. Marley RA, Swanson J. Patient care after discharge from the ambulatory surgical center. J Perianesth Nurs 2001;16:399-417.
5. Afonso AM, Tokita HK, McCormick PJ, Twersky RS. Enhanced recovery programs in outpatient surgery. Anesthesiol Clin 2019;37:225-238.
6. Temple-Oberle C, Shea-Budgell MA, Tan M, et al. Consensus review of optimal perioperative care in breast reconstruction: Enhanced Recovery After Surgery (ERAS) Society recommendations. Plast Reconstr Surg 2017;139:1056e-1071e.
7. Wheelock M, Petropolis C, Lalonde DH. The Canadian model for instituting wide-awake hand surgery in our hospitals. Hand Clin 2019;35:21-27.
8. Miller DJ, Nelson SE, Shah AS, et al. Outpatient pediatric orthopedic surgery. Orthop Clin North Am 2018;49:55-62.
9. Sevednejad N, Goecke M, Konkin DE. Timing of unplanned admission following daycare laparoscopic cholecystectomy. Am J Surg 2017;214:89-92.
10. Tan H-J, Strope SA, He C, et al. Immediate unplanned hospital admission after outpatient ureteroscopy for stone disease. J Urol 2011;185:2181-2185.
11. Duriaud HM, Kroman N, Kehlet H. Feasibility and safety of outpatient breast cancer surgery. Dan Med J 2018;65:A5458.
12. Oxley PJ, McNeely C, Janzen R, et al. Successful same day discharge after immediate post-mastectomy alloplastic breast reconstruction: A single tertiary centre retrospective audit. J Plast Reconstr Aesthet Surg 2020;73:1068-1074.
13. Lee CE, Epp A. Safety and efficiency in a Canadian outpatient gynaecological surgical centre. J Obstet Gynaecol Can 2018;40:426-431.
14. Hanley SC, Steinmetz O, Mathieu ES, et al. Safety and feasibility of endovascular aortic aneurysm repair as day surgery. J Vasc Surg 2018;67:1709-1715.
15. Goval KS, Jain S, Buterbaugh GA, Imbriglia JE. The safety of hand and upper-extremity surgical procedures at a freestanding ambulatory surgery center: A review of 28,737 cases. J Bone Joint Surg Am 2016;98:700-704.
16. Bryson GL, Gomez CP, Jee RM, et al. Unplanned admission after day surgery: A historical cohort study in patients with obstructive sleep apnea. Can J Anaesth 2012;59:842-851.
17. Mull HJ, Rosen AK, O’Brien WJ, et al. Factors associated with hospital admission after outpatient surgery in the Veterans Health Administration. Health Serv Res 2018;53:3855-3880.
18. Mull HJ, Rosen AK, Charns MP, et al. Emergency department use after outpatient surgery among dually enrolled VA and Medicare patients. Qual Manag Health Care 2019;28:191-199.
19. Van Caelenberg E, De Regge M, Eeckloo K, Coppens M. Analysis of failed discharge after ambulatory surgery: Unanticipated admission. Acta Chir Belg 2019;119:139-145.
20. ASC Quality Collaboration. Quality report. Accessed 11 July 2020. www.ascquality.org/qualityreport.
21. Alberta Health Services. Surgical contracts. Accessed 11 July 2020. www.albertahealthservices.ca/about/Page3172.aspx.
22. Dumestre DO, Redwood J, Webb CE, Temple-Oberle C. Enhanced Recovery After Surgery(ERAS) protocol enables safe same-day discharge after alloplastic breast reconstruction. Plastic Surg 2017;25:249-254.
23. Coley KC, Williams BA, DaPos SV, et al. Retrospective evaluation of unanticipated admissions and readmissions after same day surgery and associated costs. J Clin Anesth 2002;14:349-353.
24. Goldfarb CA, Bansal A, Brophy RH. Ambulatory surgical centers: A review of complications and adverse events. J Am Acad Orthop Surg 2017;25:12-22.
25. Mezei G, Chung F. Return hospital visits and hospital readmissions after ambulatory surgery. Ann Surg 1999;230:721-727.
Dr Oxley is a clinical assistant professor in the Division of Plastic Surgery at the University of British Columbia, and the Division of Plastic Surgery in the Fraser Health Authority. Dr R. Mian is a clinical assistant professor in the Division of Plastic Surgery at UBC and the Division of Plastic Surgery in Fraser Health. Ms C. McNeely is a medical student (class of 2023) in the Faculty of Medicine at the University of Ottawa. Mr Y. Mian is a bachelor of health sciences student at Queens University, Kingston, Ontario. Dr D. McNeely is a staff anesthesiologist in the Division of Anesthesia in the Fraser Health Authority.


The conclusions in the above article are predicated on two observations - that the admission rate for outpatient surgery is very low and that the readmission rate is also very low. What the study does not address is a reasonable explanation for the difference in admission rates for outpatient surgery in the setting of a hospital and that of a same-day-surgery-center? What am I missing? I suspect there is a strong bias in play!