

Pathology examination of drainage contents from thoracentesis, especially in cases of suspected malignancy, could spare patients further invasive procedures.
While vacationing in Mexico, a woman in her 70s presented to primary care with a 6-month history of B symptoms, worsening dyspnea, and new-onset back pain. Her medical history included treated ductal carcinoma in situ and a 50-pack-year smoking history. Diagnostic imaging revealed liver, lung, and bone lesions. A liver biopsy was inconclusive, identifying only an undifferentiated carcinoma of unknown primary. The woman was advised to return to Canada for ongoing investigation.
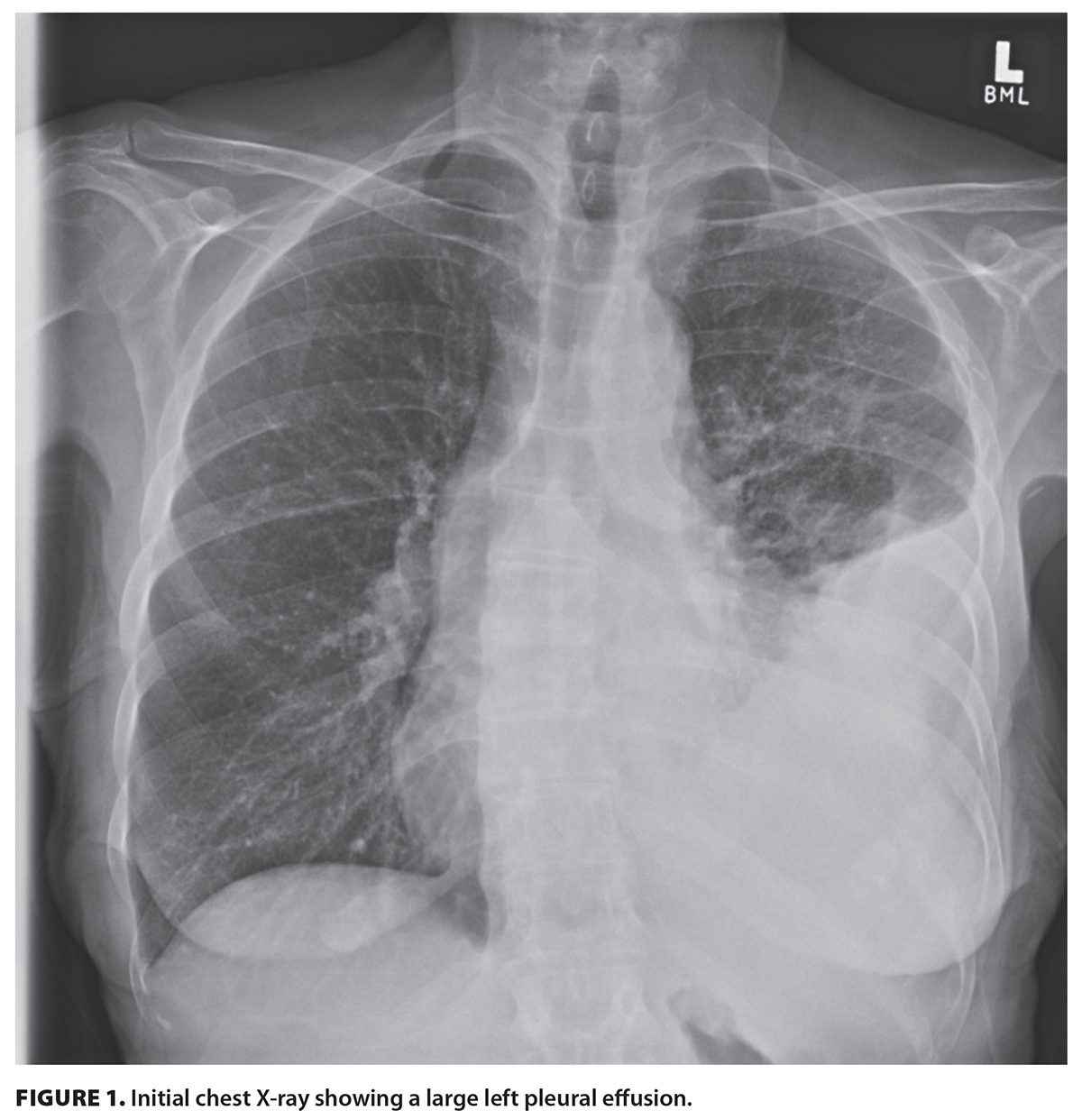
Upon presentation to a Canadian emergency department, the woman was hypoxic and minimally ambulatory. Chest X-ray showed a large left pleural effusion [Figure 1 [14]]. CT imaging showed a large left pleural effusion, multiple spiculated nodules in the left lung, mediastinal lymphadenopathy, and liver lesions [Figure 2 [15]]. Tumor markers CEA, CA 15-3, CA 19-9, and CA-125 were elevated.
 [14] [14] |
 [15] [15] |
Given these findings, a diagnostic and therapeutic bedside point-of-care-ultrasound-guided thoracentesis was performed. The imaging revealed a bulky and ragged pleural membrane at the apex of the left lung, with a consolidated lung edge floating in a hypoechoic pocket of pleural effusion with evidence of swirling debris suggestive of an exudative process [Figure 3 [16]].
After drainage of 1.2 L of serosanguinous fluid, a 3 to 4 cm globular fibrous tissue fragment was noted in the collection bag and was sent for analysis [Figure 4 [17]]. The patient’s hypoxia improved postprocedure. No pneumothorax was observed in the postprocedural chest X-ray.
 [16] [16] |
 [17] [17] |
Histopathology of the retrieved tissue confirmed metastatic pulmonary adenocarcinoma. A subsequent PET scan confirmed widespread metastases. The patient opted for palliative care and died shortly after diagnosis.
This case highlights an unusual yet valuable diagnostic outcome of thoracentesis. Tumor tissue incidentally retrieved during fluid drainage led to a rapid diagnosis, sparing the patient further invasive procedures. Proceduralists may consider pathology examination of drainage contents, especially in cases of suspected malignancy.
Consent for the use of the patient’s images was obtained from the patient’s substitute decision-maker in accordance with institutional and ethical guidelines. The substitute decision-maker provided informed consent after being fully apprised of the purpose and scope of the publication.
None declared.
None declared.
This article has been peer reviewed.
 [18] [18] |
| This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License [18]. |
Dr Ng* is a second-year radiology resident at the University of British Columbia. Dr Saleh* is a second-year internal medicine resident at UBC. Dr Wiskar is a clinical professor in the Division of General Internal Medicine in the Department of Medicine at UBC and a general internal medicine physician at Vancouver General Hospital. Dr Leung is an adjunct professor in infectious diseases at the University of Western Ontario. Dr Morrison is a clinical instructor in the Division of General Internal Medicine in the Department of Medicine at UBC and a general internal medicine physician at Vancouver General Hospital and St. Paul’s Hospital.
* Co–first authors
Links
[1] https://bcmj.org/node/10971
[2] https://bcmj.org/author/b-ng-pharmd-md
[3] https://bcmj.org/author/n-saleh-md
[4] https://bcmj.org/author/katie-wiskar-md-frcpc
[5] https://bcmj.org/author/w-leung-md
[6] https://bcmj.org/author/s-morrison-md-frcpc
[7] https://bcmj.org/sites/default/files/BCMJ_Vol67_No9_clinical-images.pdf
[8] https://bcmj.org/print/articles/incidental-tumor-retrieval-during-point-care-ultrasound-guided-thoracentesis
[9] https://bcmj.org/printmail/articles/incidental-tumor-retrieval-during-point-care-ultrasound-guided-thoracentesis
[10] http://www.facebook.com/share.php?u=https://bcmj.org/print/articles/incidental-tumor-retrieval-during-point-care-ultrasound-guided-thoracentesis
[11] https://twitter.com/intent/tweet?text=Incidental tumor retrieval during point-of-care-ultrasound-guided thoracentesis&url=https://bcmj.org/print/articles/incidental-tumor-retrieval-during-point-care-ultrasound-guided-thoracentesis&via=BCMedicalJrnl&tw_p=tweetbutton
[12] https://www.linkedin.com/sharing/share-offsite/?url=https://bcmj.org/print/articles/incidental-tumor-retrieval-during-point-care-ultrasound-guided-thoracentesis
[13] https://bcmj.org/javascript%3A%3B
[14] https://bcmj.org/sites/default/files/BCMJ_Vol67_No8_thoracentesis_Figure1.jpg
[15] https://bcmj.org/sites/default/files/BCMJ_Vol67_No8_thoracentesis_Figure2.jpg
[16] https://bcmj.org/sites/default/files/BCMJ_Vol67_No8_thoracentesis_Figure3.jpg
[17] https://bcmj.org/sites/default/files/BCMJ_Vol67_No8_thoracentesis_Figure4.jpg
[18] http://creativecommons.org/licenses/by-nc-nd/4.0/
[19] https://bcmj.org/modal_forms/nojs/webform/176?arturl=/articles/incidental-tumor-retrieval-during-point-care-ultrasound-guided-thoracentesis&nodeid=67
[20] https://bcmj.org/%3Finline%3Dtrue%23citationpop