

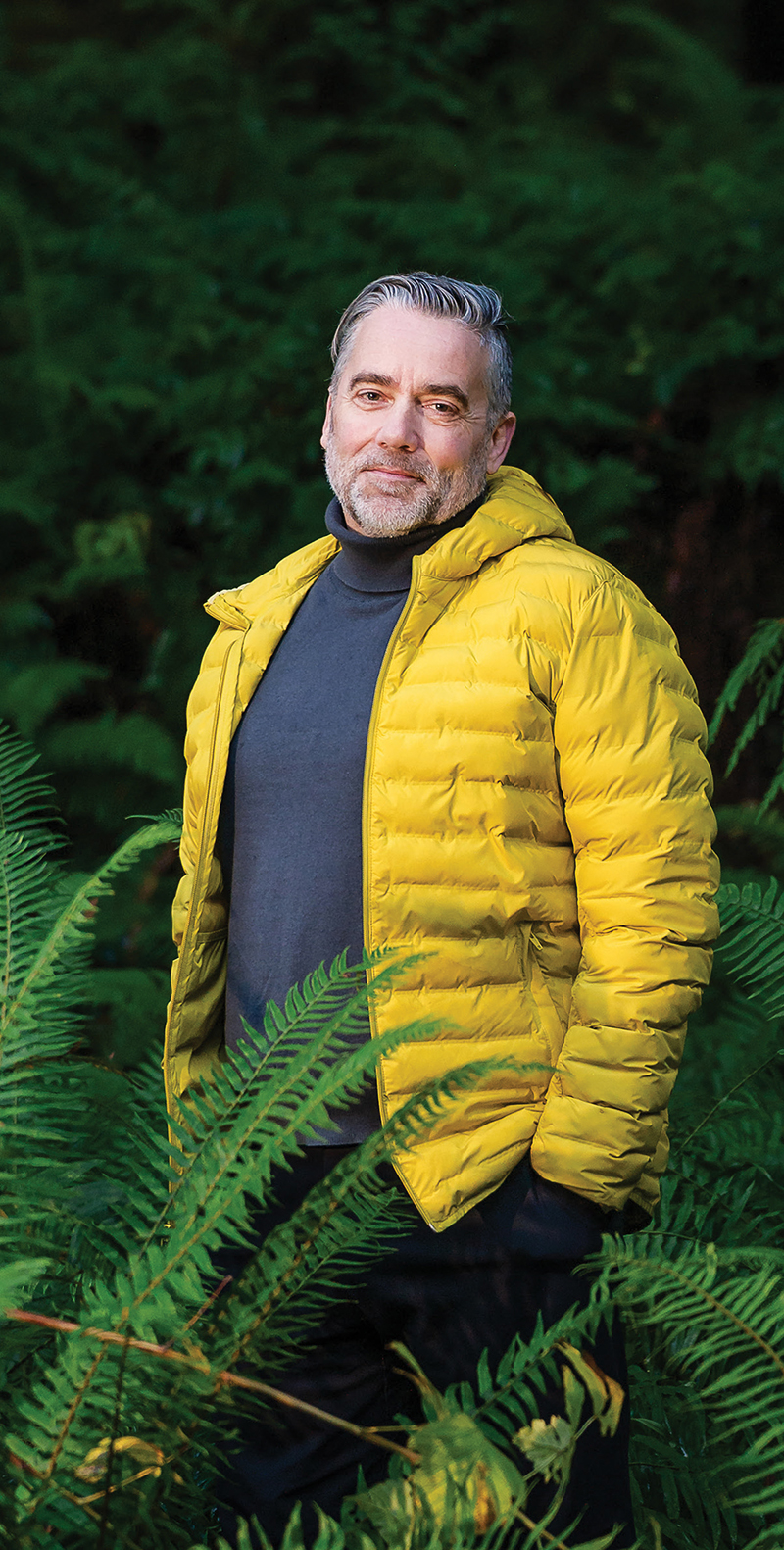
Dr Thompson, the new president of Doctors of BC, started his 1-year term in January 2026 and spoke with BCMJ editor-in-chief Dr Caitlin Dunne in December.
 [11]It’s very nice to meet you; congratulations on your new role as president of Doctors of BC. For our readers who don’t know you yet, perhaps you’d like to start with an introduction.
[11]It’s very nice to meet you; congratulations on your new role as president of Doctors of BC. For our readers who don’t know you yet, perhaps you’d like to start with an introduction.
I’m Adam Thompson, a family doc in Courtenay, on Vancouver Island. I’m married to Emma, a psychotherapist, and we have two boys. We moved here from the UK in 2011. The boys are now both at UBC Okanagan, following two different paths. One is possibly heading toward medicine—we’ll see. He’s doing a bachelor of neuropsychology at the moment. The other is doing a bachelor of digital media, and he’s head of sports photography at UBC Okanagan—he wants to become a sports photographer.
And you have a busy, full-time family practice in Courtenay. How did you balance career and family after you immigrated?
I made sure to protect space to be with my family, the boys in particular. It’s important that boys have a positive male role model when they’re growing up, projecting the caring side of masculinity. My wife and I made sure to take time away from work on the weekends when we could—we’d go skiing or biking together, or even down to the pub as the boys grew up, just to spend intentional time and be present. Our jobs are busy—we all know that—but there is an interdependency between all the spaces in which we exist, meaning that work has to give way to other parts of life at times.
More than anything, our families—and family can mean whatever you want it to mean, whatever your place of comfort is—are what ground us in the work we do as physicians. And I believe we need to be humans first across all aspects of our life—family, friends, and community; in our professional role; and particularly in leadership.
I agree. As a fertility doctor, I find myself telling people every day that there are many ways to build a family. What did your family think about you wanting to take on the job of president of Doctors of BC?
We’re always supportive of anything any of us wishes to try to achieve. With Emma being a psychotherapist, we spend a lot of time talking; communication is key. The boys are excited that I might be popping over to Kelowna occasionally because of work, so there’s an opportunity to connect and catch up. Emma understands that I’m going to be away more, but at the same time, there will be opportunities for her to be with me at some events, and we’ll be chatting often. She’s fully supportive, as was I when she chose to do a master’s degree in psychology. That, for me, is the value of family: it’s the foundation from which we can go out and explore the world.
Tell us about some of your observations or learnings from your role as president-elect over the past year.
I can’t remember the last time someone came from the Board to become president. I’ve been vice-chair and chair of the Board, I led the organization through leadership change, I led the development of the current strategic plan, and I was involved in developing the Longitudinal Family Physician (LFP) Payment Model, so I’ve been quite immersed within Doctors of BC. Presidents-elect have often come from outside the organization, or certainly outside the Board, so they spend a lot of time learning initially. To some extent, I didn’t have to spend the year learning in that way, so I could ensure I was present at the Board as a contributing director.
The biggest opportunity I had was to be more exposed to physician wellness and the current physician wellness crisis. We know that when students enter medicine, they have better psychological health than their peers. And yet, by the end of their residency, they’re quite unwell. We’re all suffering.
One thing that struck a chord with me, having grown up in Britain and worked there for something like 15 years, is the concept of institutional professionalism—the desire to conform to and assimilate into our career and present ourselves in a certain way, with our white coats. You certainly wouldn’t show your tattoos or piercings or the other side of who you may be.
By attending various physician wellness events and some rural events, and through some of the truth and reconciliation work we did as we formed the Guiding Circle at Doctors of BC, I learned the commonality in need and purpose from these various spaces—that it’s about who we are as people that connects us and allows us to have the difficult conversations. I also learned that I quite enjoy sound baths and floor yoga. Who knew!
I want to be seen as the same person in leadership as at home, in the office, and so on. Let’s get rid of the hierarchy, assimilation, and conformity that our profession sometimes demands of us. I think physicians do extraordinary things, but they’ve also got families, they’ve got vulnerabilities, and they’ve got stressors, and the more we can connect with each other as people first, the better able we’ll be to support one another in this profession.
I get great pleasure out my job as a family doctor through the connections I have with my patients. Connecting is the secret sauce of the work we do as physicians, and it’s what I think we need to do as leaders.
I want to touch on the LFP Payment Model. I am not a family physician, but from what I have heard and read, by many accounts, it’s been very well received. I think it has also struck up conversations across the country about how family physicians are remunerated. I’ve heard from many family physicians who have corresponded with the BCMJ that this has brought a boost of optimism to what could arguably be described as a bleak situation for many doctors, especially family doctors. What do you see on the horizon that might provide some light, some optimism for family doctors or BC physicians in general, who are struggling with workload, low morale, or burnout?
That’s a difficult question, because we are in difficult times.
It’s worth remembering that the payment model came from patient pressure on the government and political pressure from the government. I’d love to big-up the fact that as medical leaders at Doctors of BC we were being phenomenal advocates and did a great job, but in reality it was political pressure on the government, patients on the legislature lawn—acknowledging that BC Family Doctors and BC College of Family Physicians leaders may have supported that. Doctors of BC, by cultivating a collaborative relationship with the government over the years, was in a place where the government could come to us for help and support to develop that payment model. I hope the government remembers that the intent was to stave off a forthcoming crisis, more so than to reform and improve primary care. We have an eye on that, and there’s still a pathway to improve primary care further than the LFP Payment Model has already—if the government works with us appropriately, and if the government uses the levers appropriately to drive the issues it wants. We devised the model with the intent to improve attachment, to improve access.
We are facing a difficult time—it’s no secret that the government is billions of dollars in deficit, that we have significant reviews going on in the health care system, where the government is looking for financial reforms. One thing I look to with positivity is that when we hit periods of change like I think we’re going to hit, it always brings opportunity. We’ve got to be alive to the potential to revamp and reform the health care system. We have phenomenal staff at Doctors of BC, incredibly thoughtful and dedicated to the work they do. We have some great leaders too. The light for me is maintaining Doctors of BC in the space where we can work with the government to try to help it solve problems moving forward. There are fires all over the province. We’ve seen a number of challenges of physicians struggling to provide services. I think there are challenging times ahead, unfortunately. The light that I see is in the power we have to connect with each other, band together, support each other, and seek opportunities as they arise.
Through the LFP Payment Model, we did something for primary care, and we’ve been battling ever since to do something for specialist care. We’ve struggled to get the traction we need to improve that situation. I’ve seen the pressure of wait lists and the pressure of not having team-based care to support specialists in their work by working alongside a consultant dermatologist in my office. I know this from other leaders in the specialist space as well, and we’ve got to maintain the strength of being together to advocate, to effect the change.
There is still a major shortage of family physicians in BC, and there are a number of initiatives aimed at trying to get more medical students to choose family practice—we have the SFU School of Medicine starting to accept students in 2026. And your son is potentially heading toward a career in medicine. What would you say to inspire him to choose family practice in this environment?
If my son chooses a career in medicine, I’ll support him in whichever direction he chooses. I have a suspicion that, if anything, he’ll try to become a neurologist.
We need more of literally every specialty across medicine. That’s the bottom line. As an example, as a family doc, I cannot get dermatology care on the island, as our dermatologist is leaving. I’ve got to do virtual contacts or rely on the RACE line or send people to Vancouver. We need physicians across all disciplines.
There are opportunities, though. We’re right to try to recruit from the US. I’m currently in dialogue with one US physician looking to move to a different system and perhaps somewhere they feel more culturally aligned.
I was speaking with a friend’s son who is now a doctor about to graduate residency in the UK, and they can’t get jobs over there because of the way the system is being funded. So there’s an opportunity to bring over more UK grads as well.
To inspire anybody into medicine is to talk not only about the intellectual stimulation, but also about the value you get from delivering care well and the satisfaction of improving somebody’s life as a result.
When I was a young doctor starting out in primary care in England, we used to do an on-call system where two docs would be on in the evening with a couple of nurses, for a population of about 200 000, and we’d sit around in the evening chatting and drinking coffee to keep us up. I was chatting with one doc, and I vividly remember him saying, “Adam, in general practice, we sort of nudge things along a bit, but ultimately, we don’t often change the medical path of what’s happening to the patient. They’re still going to experience illness. Our job is to make them as content and as happy as possible along the journey.”
That stuck with me as the important part of being a family doctor—being there as the advocate, being there to support patients. It’s about the privilege of being in a position to care, to look after someone, and to make their health a bit better on that journey.
 [12]You took on a leadership role early in your career, as a resident; there have probably been some highs and some lows in your evolution. Tell me about that journey.
[12]You took on a leadership role early in your career, as a resident; there have probably been some highs and some lows in your evolution. Tell me about that journey.
First, I’m not an academic leader, and I haven’t done any of the big leadership courses. I am a completely experiential learner, both from other leaders, spaces, sources, and observations, and from having deep, rich conversations with people. There is something innate in the makeup of all medical leaders that keeps driving us. I think the work I’ve done and the journey I’ve had in leadership shows you don’t necessarily have to rely on that academic side to progress.
My first leadership experience was in residency. I was doing a 1 in 4 on-call in the UK; we would start at 9 a.m. on Saturday and finish at 5 p.m. on Monday, and there were two juniors. We split the Saturday and Sunday nights and had 4 hours’ sleep each. One of us had noon until 4, and the other had 4 until late. Other than that, we just worked solidly. We were getting half pay while doing that, which was mildly insulting.
It was clear we had a case to make as a group of physicians that we should be getting full pay for the hours we were working. To me, it was basic justice, to be honest, which is a crucial leadership value for me.
So, I corralled my colleagues, we filled out some time-management diaries, and I presented the case to the British Medical Association rep and the hospital board and said, “You owe us money.” They ended up paying us, and that was my first experience in leadership.
Probably 5 or so years later, I was working in my hometown of Worcester, and the government tried to introduce private providers into the primary care space in the National Health Service (NHS) through a commissioning process.
Our city was to be one of the places where they would put out a tender for a new model of primary care. All the clinics and doctors were up in arms, ready to wave placards, saying, “This is terrible; how can you bring in private care?” Ironically, as independent practitioners, we were all private anyway, but on a much smaller basis than any of the big companies looking to come in.
We had a meeting with about 100 doctors, and everyone was talking about how to protest, how to resist, and I stood up and said, “We can protest all we like, and we’ll feel better for it in the short term, but we can’t change this coming, so why don’t we think about how we can get together as a group of doctors, build something that would enable us to bid for this, and see whether we can harness it for the good of us all and our community?”
I sat down, expecting people to say either “You stupid idiot” or maybe “That’s an idea; okay, we’ll take that forward.” Instead, the senior heads in the room went quiet, and then one of them stood up and said, “That’s a good idea, Adam. Can you get on and do that, then, please?”
I was rougher around the edges back then, but I got on with it. I learned a lot from my brother-in-law at the time, who was a tax/corporate lawyer. He and I would sit at football matches and talk about legal structures. From that I built a limited company, and I persuaded 64 other family doctors to invest in the vehicle we built. I worked collaboratively with one of the local health authority provider trusts to build a bid and a tender. It was ridiculous; I was working 16-hour days, 7 days a week, for 4 or 5 months—full-time primary care and the rest of my time writing up this tender and this bid. But we won the contract.
We started to provide the service, and it did really well. The community received it well, and primary care physicians were happy that it was in our control, so there was no resistance from local clinics.
But the UK NHS changes its politics every 5 minutes, and it wanted to do something different again. At the time, I was less able to manage my frustrations around how it was changing. This is a skill I’ve since learned—understanding and holding on to the pragmatic reality that things change and you have to adapt.
I wanted to step away from leadership, maybe for a period of reflection, and then other things transpired in our lives, and we decided that we wanted to move somewhere where we could grow as a family—we didn’t feel a strong connection to the UK. I vowed when we moved here that I wouldn’t get involved in medical leadership again, because I felt a bit burned from it.
As part of moving here, I had to do exams in the UK, LMCC I, LMCC II, and all the rest of it, along with getting to know the system and re-upskilling in hospital care. But my next-door neighbor was vice chair of the Comox Valley Division of Family Practice, and as happens in small communities, he had us over for a meal and a chat, and I told him about my leadership work, and he said, “Oh, you should really apply for the Board.”
I looked into it and applied, and when he stepped away from being vice chair, someone said, “Well, you really ought to be vice chair.” I said, “Oh, okay.” And eventually the chair stepped away, and someone said, “You really ought to be chair.” And so I was back into leadership. The great thing about being in the division, as opposed to my role in the UK, is that our division was very well set up, and I worked closely with our executive director—somebody I learned from, Janet Brydon, a wonderful person.
She and I decided to go to town trying to get a primary care network (PCN) up and running, working alongside Dermot Kelly—who was an Island Health executive at the time but is now president and CEO of Fraser Health; we positioned Comox to be one of the first five in the province. We worked collaboratively with other PCNs and Dr Charlene Lui, who was in Burnaby at the time. We had a number of meetings of those five divisions. We had meetings with the ministry. We put heart and soul into trying to drive this to a place of success. There was a real opportunity to support family medicine with better team-based care and provide an environment that would better support physicians, as well as provide for attachment and provide for a community I chose to live in. As an immigrant, I have a great sense of wanting to pay back the community.
Unfortunately, what the ministry decided the PCN was going to look like was nothing like what many of our divisions wanted it to look like. It was a cookie-cutter approach, a health authority–dominated model without any of the things we wanted to develop—embedding it into the community of physicians, having strong community ownership, having the flexibility that physicians needed, and most importantly having physician leadership. Physicians know what their communities need, and this model didn’t provide that. When we had the opportunity to speak with [Adrian] Dix, health minister at the time, I raised my concerns about the PCN model, which led to him ordering a PCN refresh process with the support of the Family Practice Services Committee.
Frustration, irritation, and perhaps a bit of burnout from working hard to achieve something and having the result not be quite what I envisioned made me think about seeking an exit strategy and encouraging someone else to take on the role. After I slowly slipped out, I thought that might be the end of my leadership career.
Then, a division of family practice colleague of mine on the Island, who was on the Representative Assembly, encouraged me to run for a Board director position at Doctors of BC.
I thought about it, and one of the things I was concerned about through the PCN process was the way Doctors at BC was advocating for physicians with the government. I wanted to understand why we’d landed on a model that physicians didn’t want—not what Doctors of BC’s culpability was on that, but what was going on with our advocacy that had partly led to that.
I’ve come to learn that the Ministry of Health has the legislative pen, it holds the budget, and if the ministry wants to legislate, it can. We’re seeing this in Quebec and Alberta. But how can we better advocate to ensure we have a system that physicians want to work in and feel comfortable working in? Because when we’re all right, our patients are all right.
Shortly after I joined the Doctors of BC Board, we were hit with the pandemic, which led to major stress for the profession and for the Board. Frankly, we became a little divided around a senior leadership issue, which made it an even more challenging time. In the end, the Board decided to shift senior leadership within the organization, which was a difficult decision, but I believe it was the right one, and I think we’ve borne that out. I was then encouraged by a section of the Board to become chair, and as chair, I recognized that we needed to better connect physician leadership within and outside of Doctors of BC, because for far too long, we operated in silos. And when we’re in silos, we’re at higher risk of squabbling or being competitive. Physicians are competitive; that’s the bottom line, but we need to apply it to achieve something together.
Because I wanted to build things back together, I designed a Board retreat away from our usual space, and we brought in the Joint Collaborative Committees co-chairs, to come together with human connection, and also kick off the beginning of the strategic plan, and we built the idea of regular Better Together meetings. We’ve maintained that group and added the societies, and I think it will evolve over time.
And of course, the opportunity for the LFP Payment Model came up, and it was an honor to work alongside four other great leaders: Dr Ramneek Dosanjh, who was Doctors of BC president at the time; Dr Joshua Greggain, who was president-elect and connected well to rural; Dr Maryam Zeineddin at BC Family Doctors; and Dr Renee Fernandez at BC Family Doctors.
Dr Fernandez and I co-led the process of negotiating to deliver something for our primary care colleagues. Doctors of BC, and the Board in particular, have worked hard ever since to try to deliver something for specialist care colleagues, particularly around the wait list initiative, which we’ve been working on since 2023. For whatever reason, the government isn’t yet acting on our advocacy alongside Consultant Specialists of BC. It is an issue we need to continue highlighting.
Fairness and equity are important values to you, and Doctors of BC has been a leader in its strategic plan and in committing to improvements in cultural safety, anti-racism, and Indigenous-led initiatives. What does that mean for your presidency, for physicians, and for equity-deserving patients in BC?
We have stood up our Guiding Circle at Doctors of BC, and as president, that’s something I will be a part of. We want our Indigenous colleagues and partners, both physicians and nonphysicians, to be very visible. It’s through visibility and understanding that we drive reconciliation. I believe that truth and reconciliation must ensure that all truths are heard to get to a point of reconciliation. Sitting down in guiding circles and understanding each other’s perspectives will be key in the next year. I want to see how we drive our Guiding Circle to help inform Doctors of BC across the organization and across policies, not only valuing and uplifting Indigenous communities and the care of Indigenous patients and supporting Indigenous physicians in their work, but also bringing aspects of Indigenous culture into the work we do. When I sit with Indigenous friends, or in something like the Guiding Circle, it’s always led with “Who are you as a person?” We can learn a lot from Indigeneity about how to show up with each other. I want to reflect some of that this year, and I want to make our Guiding Circle more visible to members. I also want our members’ truths about how they feel about truth and reconciliation to be heard, because there’s a diversity of views, and we need more than a unipolar approach. We have to understand how everybody is feeling to get to points of reconciliation.
When I was Board chair, we also stood up the IDEA (Inclusion, Diversity, and Equity Advisory) Committee to look at how we could do better in terms of EDI, both within Doctors of BC and within the profession. For instance, I still see a significant gender imbalance in medicine. Dr Dosanjh was recently appointed executive vice president, North America, for the Medical Women’s International Association. It’s exactly the space that she will be excellent in—tenacious and fearless—and maintaining connections such as this as president will enable me to better understand some of the gender imbalances that we experience.
If we go back to the principle of showing up as people first, people are diverse, and we need to ensure everybody feels comfortable showing up as who they are. Otherwise, we’re not tapping into the full talents of humanity. I’m cognizant that I am a white, middle-aged male, growing up through a patriarchal profession, and that my own projections of who I am could be offensive to some people, particularly with my stern British accent and stiff upper lip and all that. I hope that trying to lead as a human first will ensure that people see that we’re all in it together.
You have a lot of great ideas and experiences to help inform your goals for the year ahead. Are there any other causes you’re interested in pursuing that we haven’t touched on yet?
I’m very keen to advocate that we have a responsibility to do something about climate change. As physicians, our role is to care for society and the community, and I believe one of the biggest threats to society and communities is climate change. We have a responsibility to try to offer leadership in that space.
When your presidency is finished, what would be a mark of success for you in this role?
My role is to be a representative of the profession—the spokesperson for the organization and potentially the spokesperson for physicians. The Board’s role is to set the direction for how Doctors of BC functions and its policies and strategy. That’s important to remember.
I hope people see me as having demonstrated an ability to fight for them, but in a compassionate way. If I can persuade physicians that it’s okay to show up as they are, rather than feeling they have to put on the armor of a white coat and assimilate, then I will feel that I have achieved something. I also want to focus on ensuring that we see leaders as just other humans doing the job alongside our colleagues.
hidden
 [14] [14] |
| This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License [14]. |
Links
[1] https://bcmj.org/cover/januaryfebruary-2026
[2] https://bcmj.org/author/caitlin-dunne-md-frcsc
[3] https://bcmj.org/node/11060
[4] https://bcmj.org/sites/default/files/BCMJ_Vol68_No1_interview.pdf
[5] https://bcmj.org/print/interviews/dr-adam-thompson-connection-above-all-else
[6] https://bcmj.org/printmail/interviews/dr-adam-thompson-connection-above-all-else
[7] http://www.facebook.com/share.php?u=https://bcmj.org/print/interviews/dr-adam-thompson-connection-above-all-else&via=BCMedicalJrnl&tw_p=tweetbutton&via=BCMedicalJrnl&tw_p=tweetbutton
[8] https://twitter.com/intent/tweet?text=Dr Adam Thompson: Connection above all else&url=https://bcmj.org/print/interviews/dr-adam-thompson-connection-above-all-else&via=BCMedicalJrnl&tw_p=tweetbutton&via=BCMedicalJrnl&tw_p=tweetbutton&via=BCMedicalJrnl&tw_p=tweetbutton
[9] https://www.linkedin.com/sharing/share-offsite/?url=https://bcmj.org/print/interviews/dr-adam-thompson-connection-above-all-else&via=BCMedicalJrnl&tw_p=tweetbutton&via=BCMedicalJrnl&tw_p=tweetbutton
[10] https://bcmj.org/javascript%3A%3B
[11] https://bcmj.org/sites/default/files/BCMJ_Vol68_No1_interview_Dr-Adam-Thompson-1.jpg
[12] https://bcmj.org/sites/default/files/BCMJ_Vol68_No1_interview_Dr-Adam-Thompson-3.jpg
[13] https://bcmj.org/sites/default/files/BCMJ_Vol68_No1_interview_Dr-Adam-Thompson-2.jpg
[14] http://creativecommons.org/licenses/by-nc-nd/4.0/
[15] https://bcmj.org/modal_forms/nojs/webform/176
[16] https://bcmj.org/%3Finline%3Dtrue%23citationpop